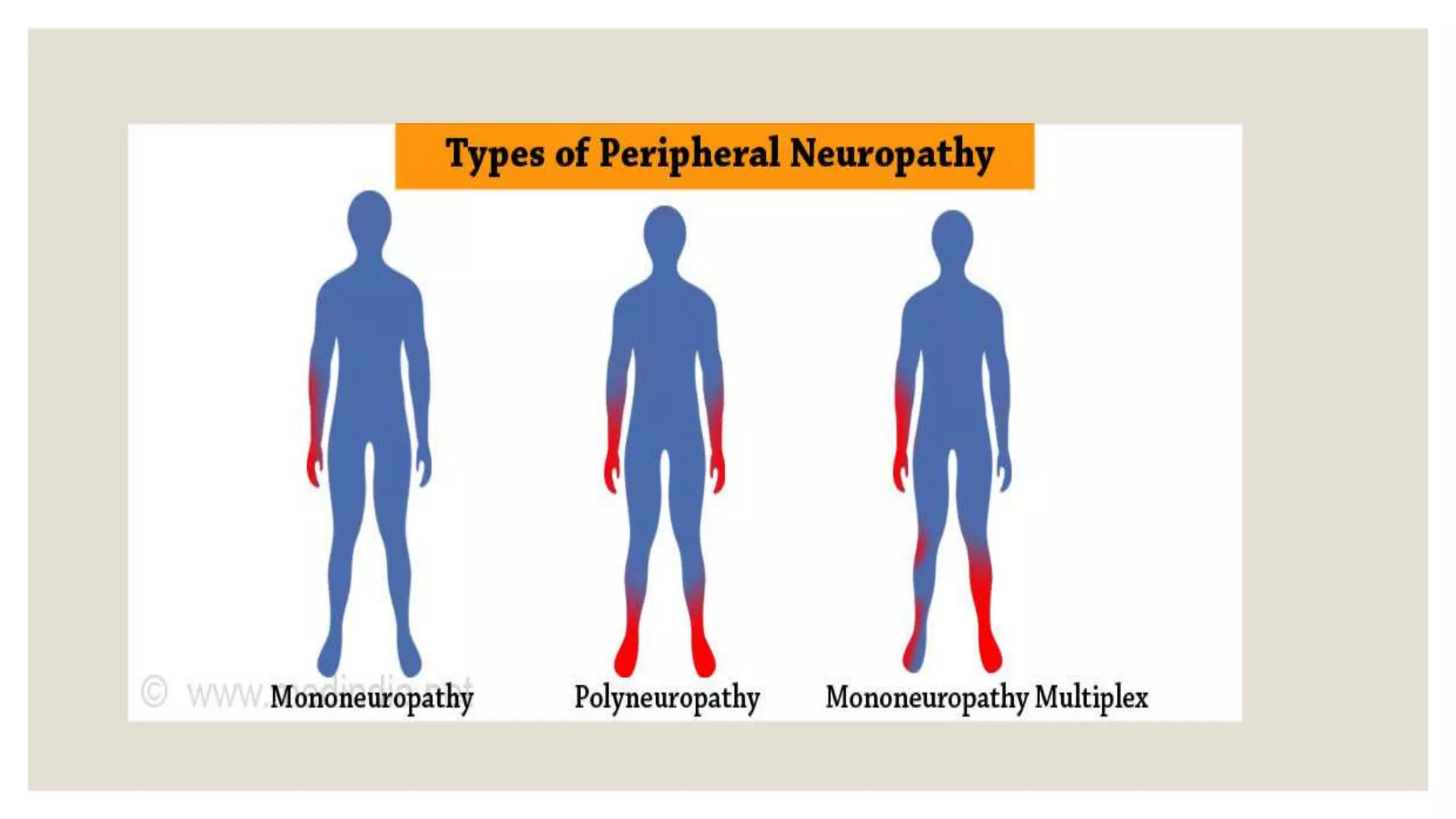
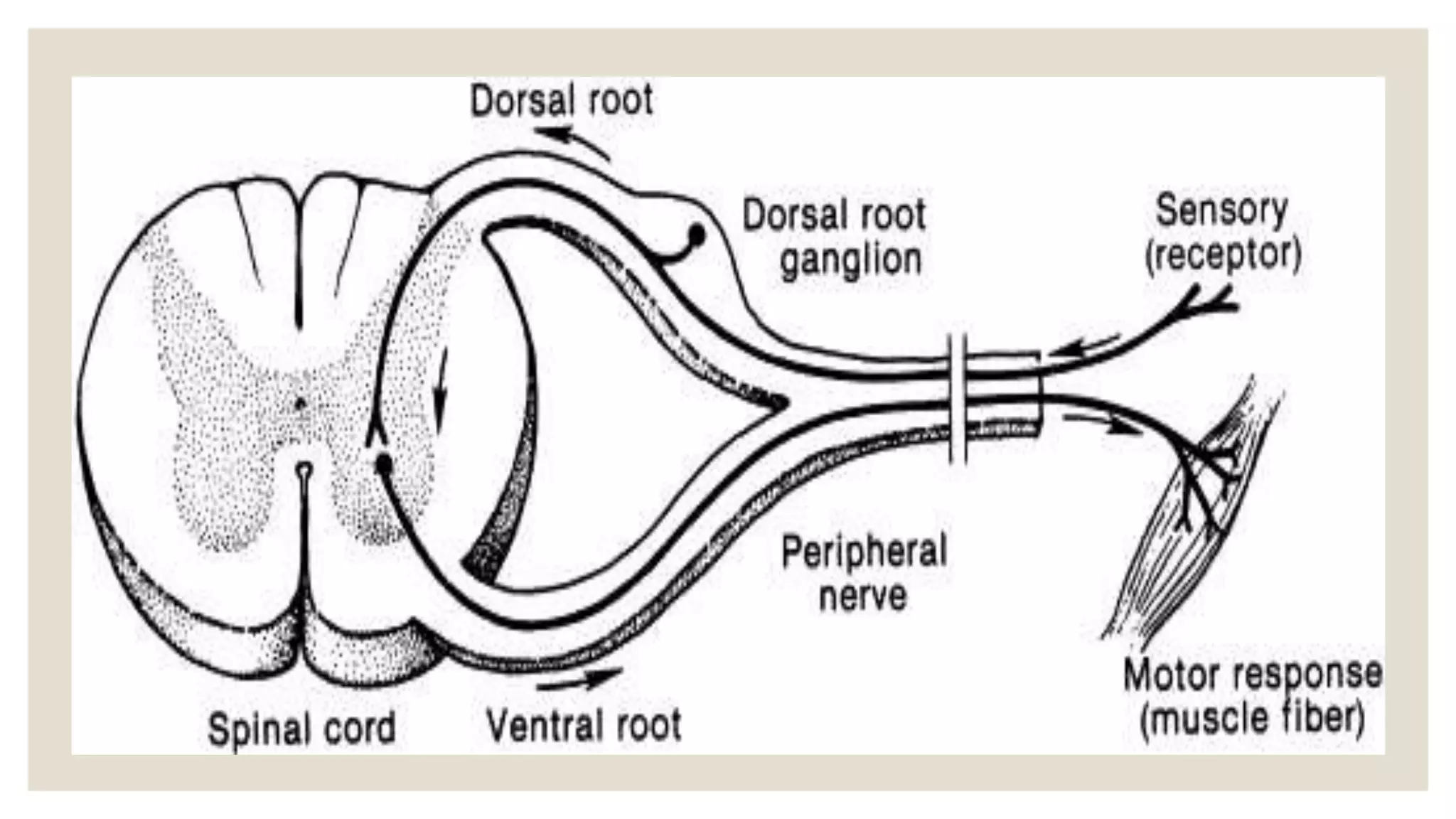
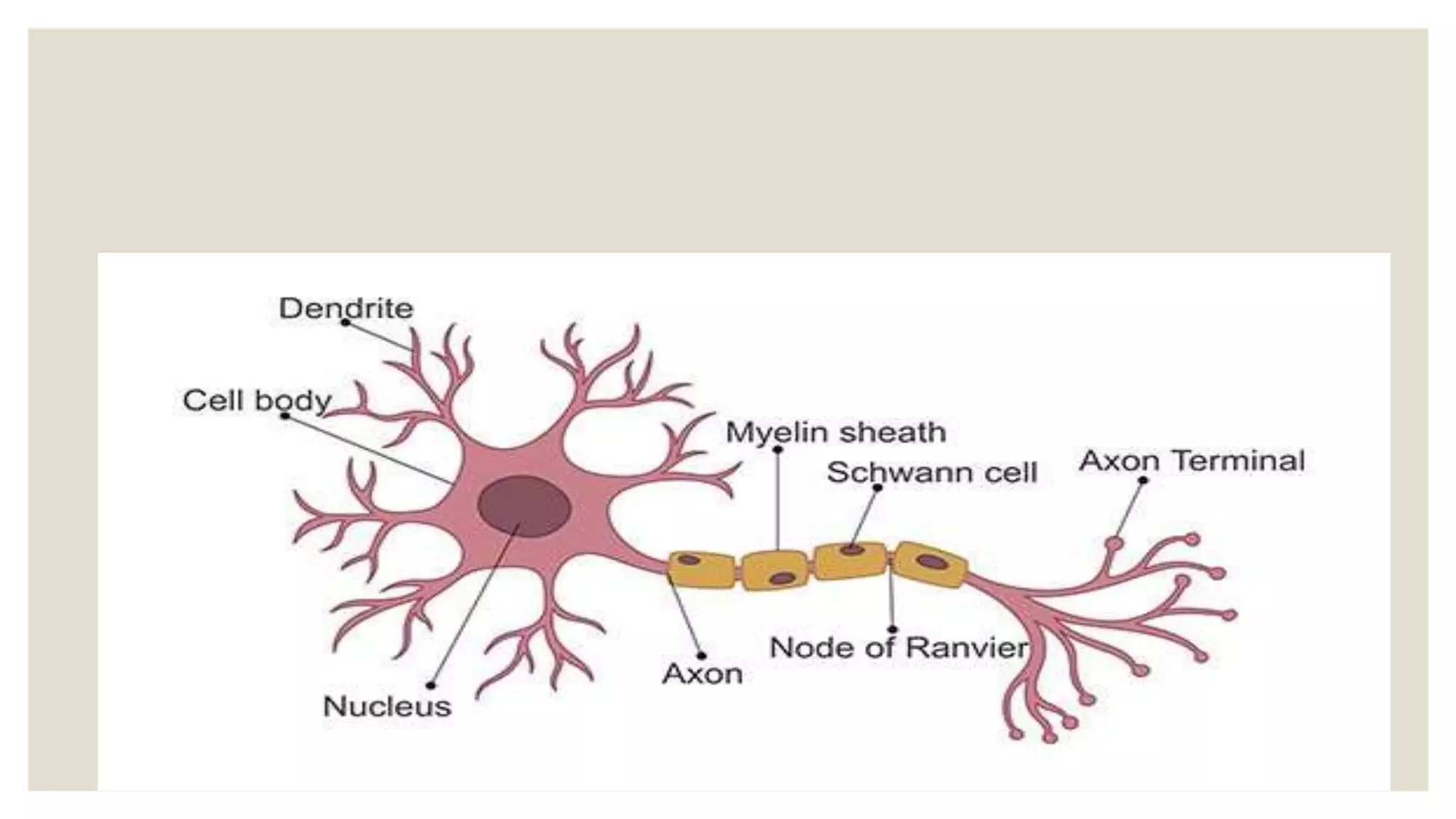
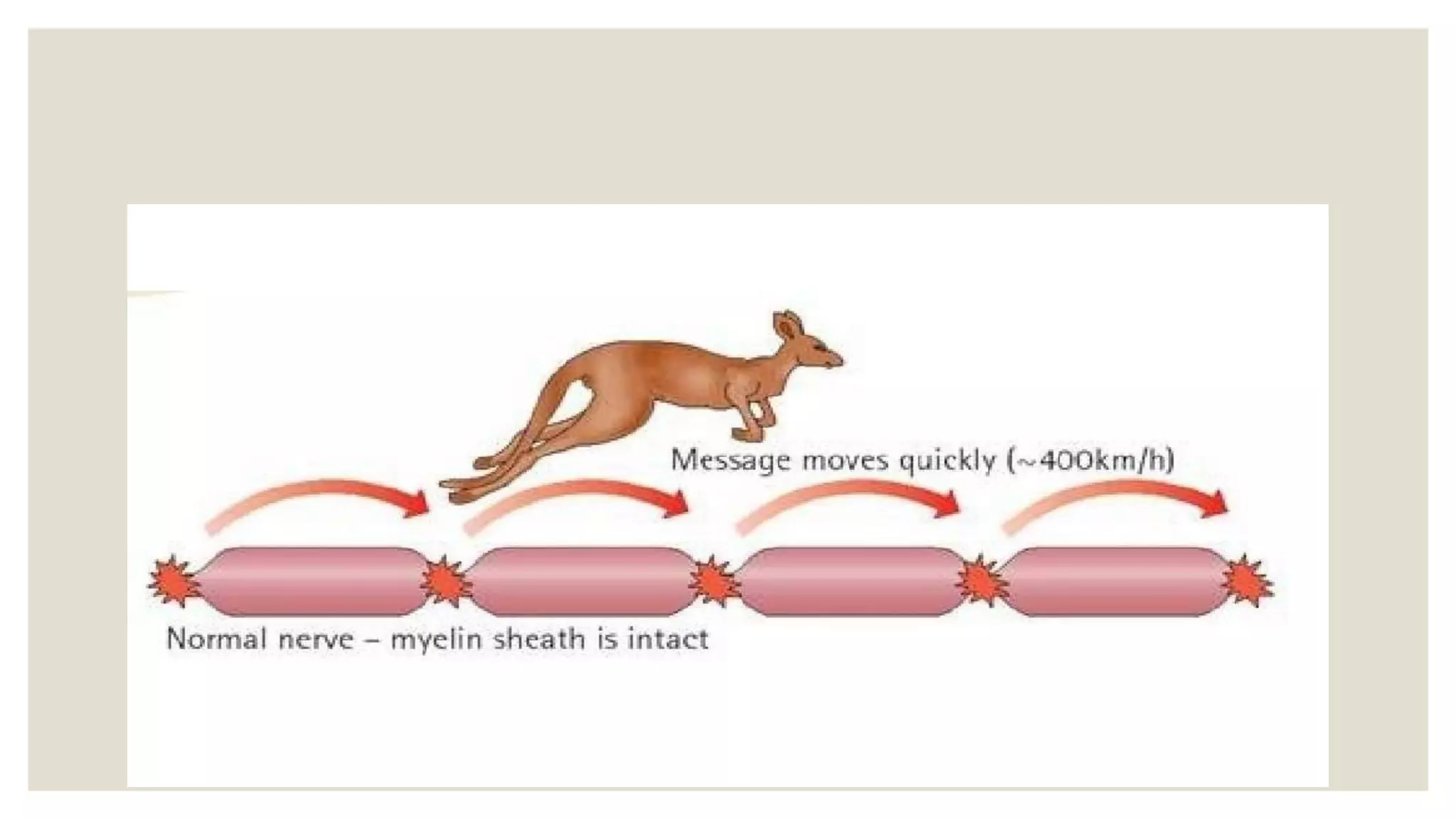
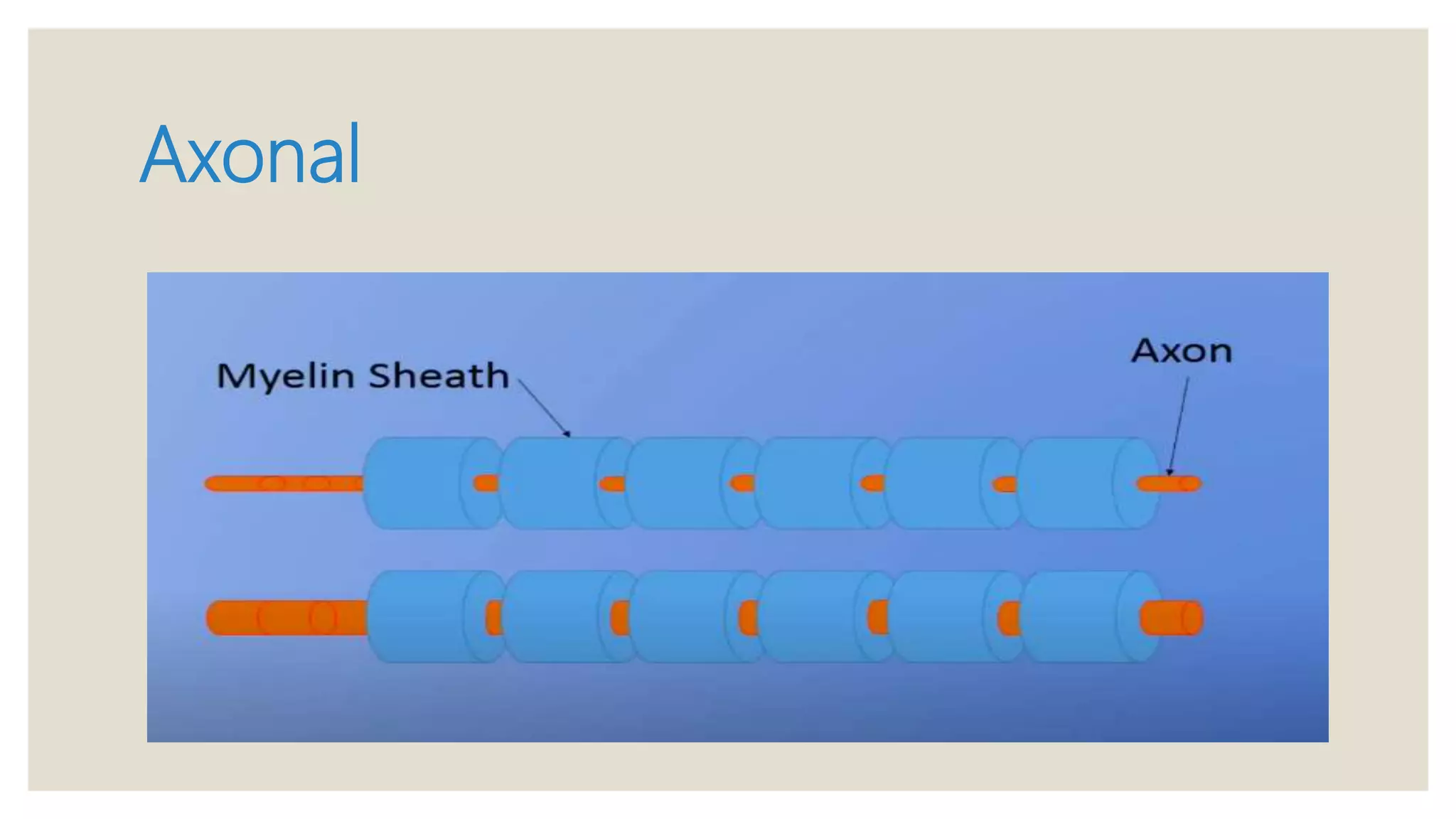
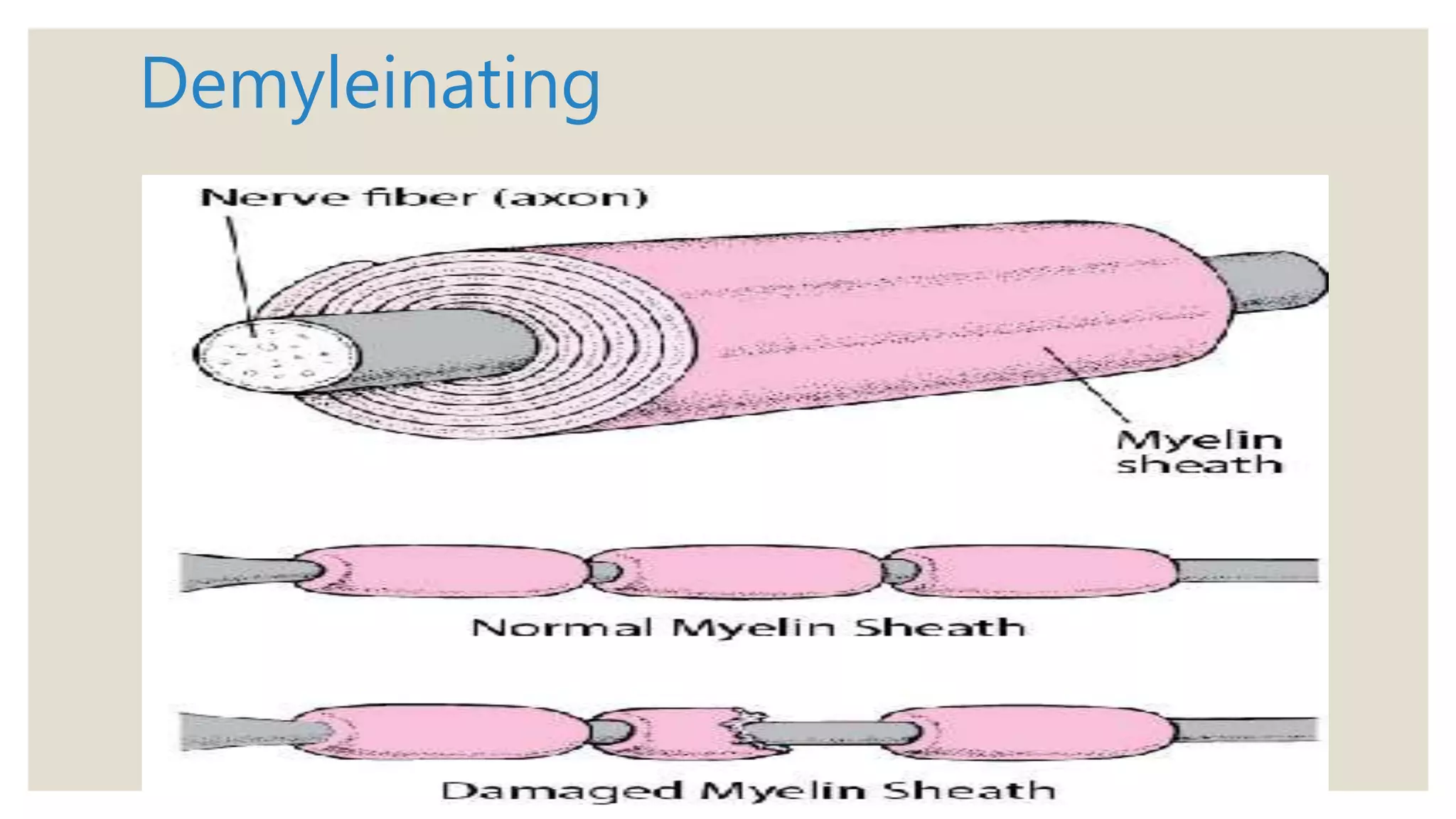
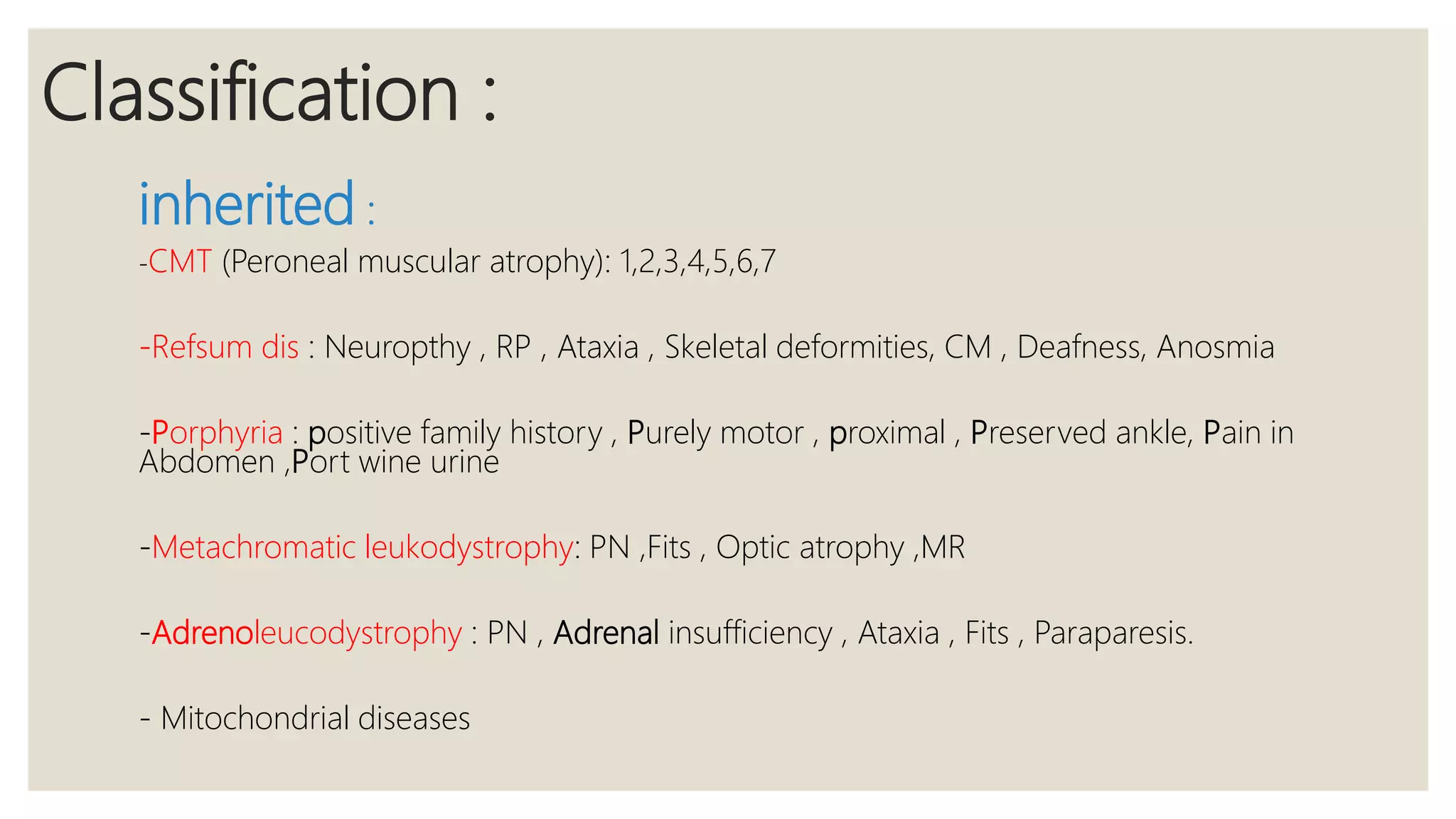
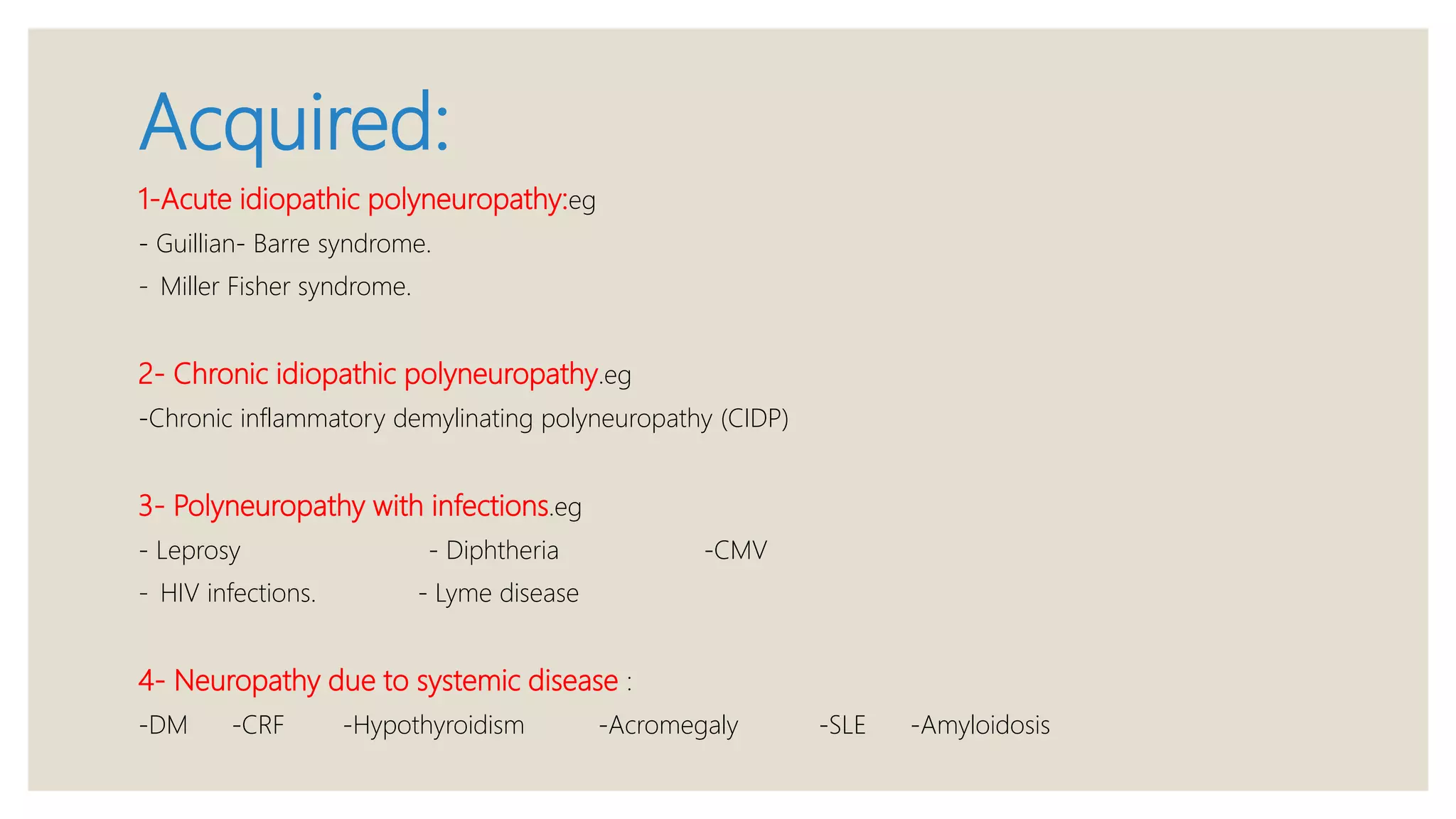
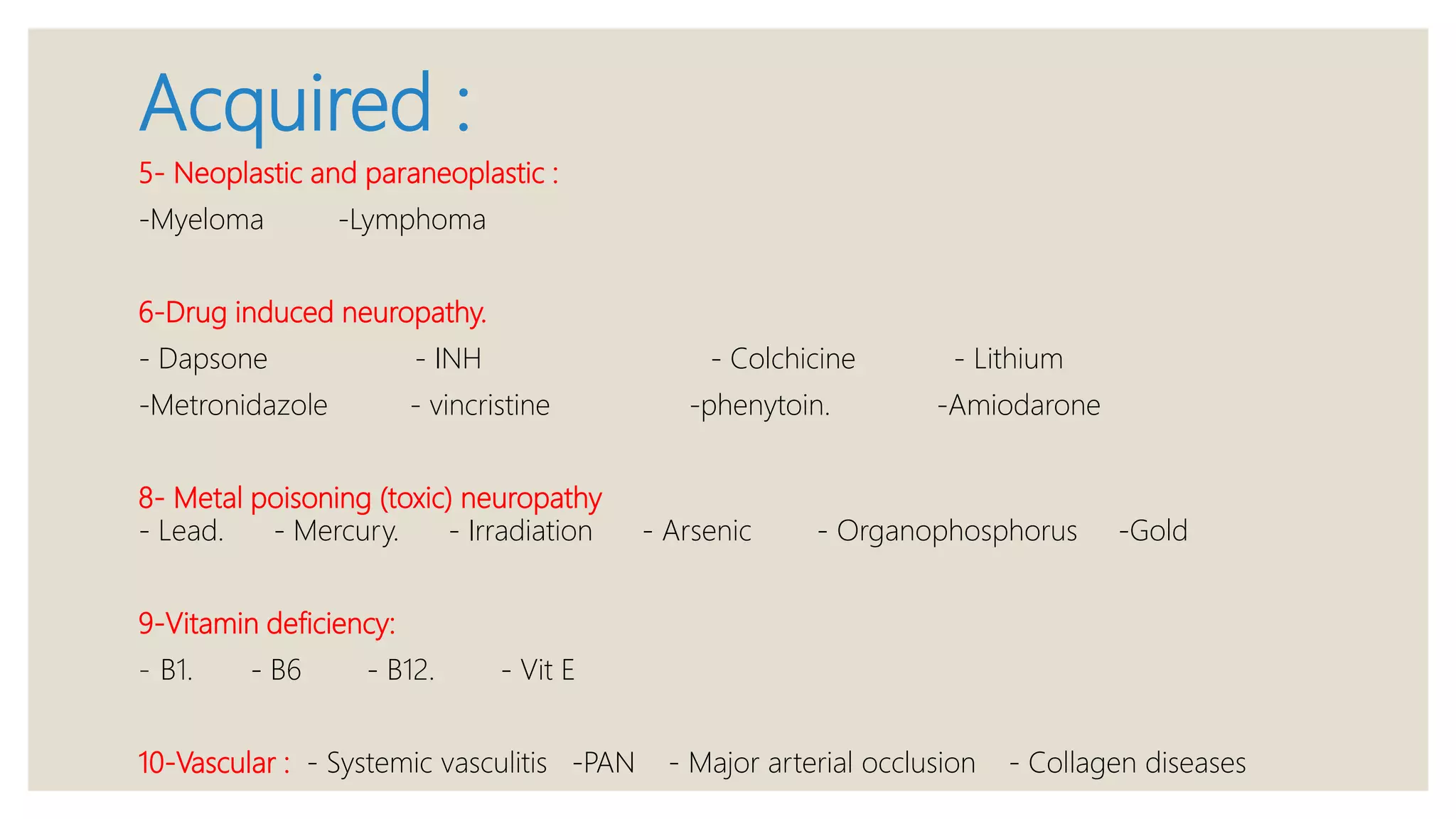
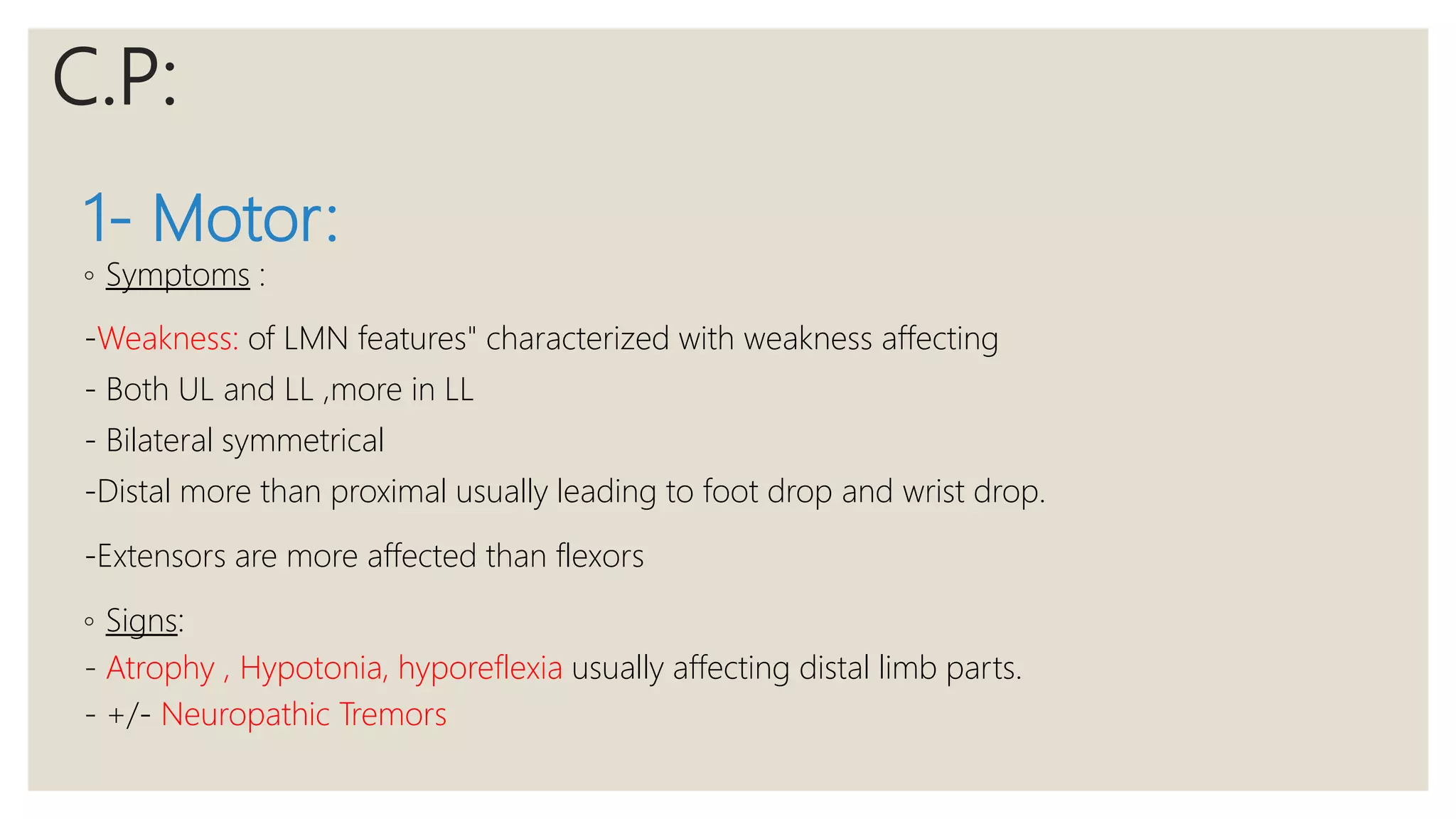
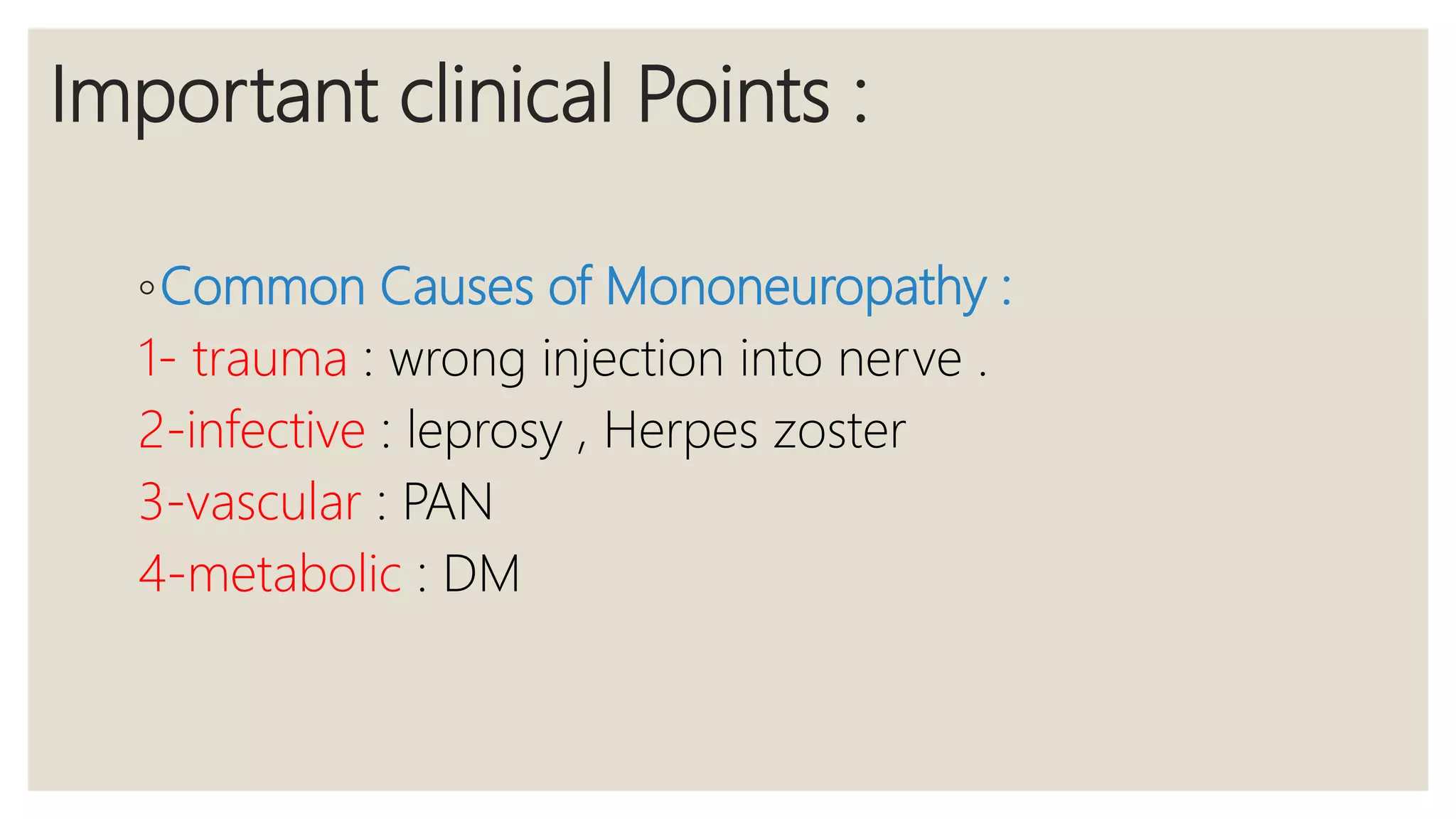
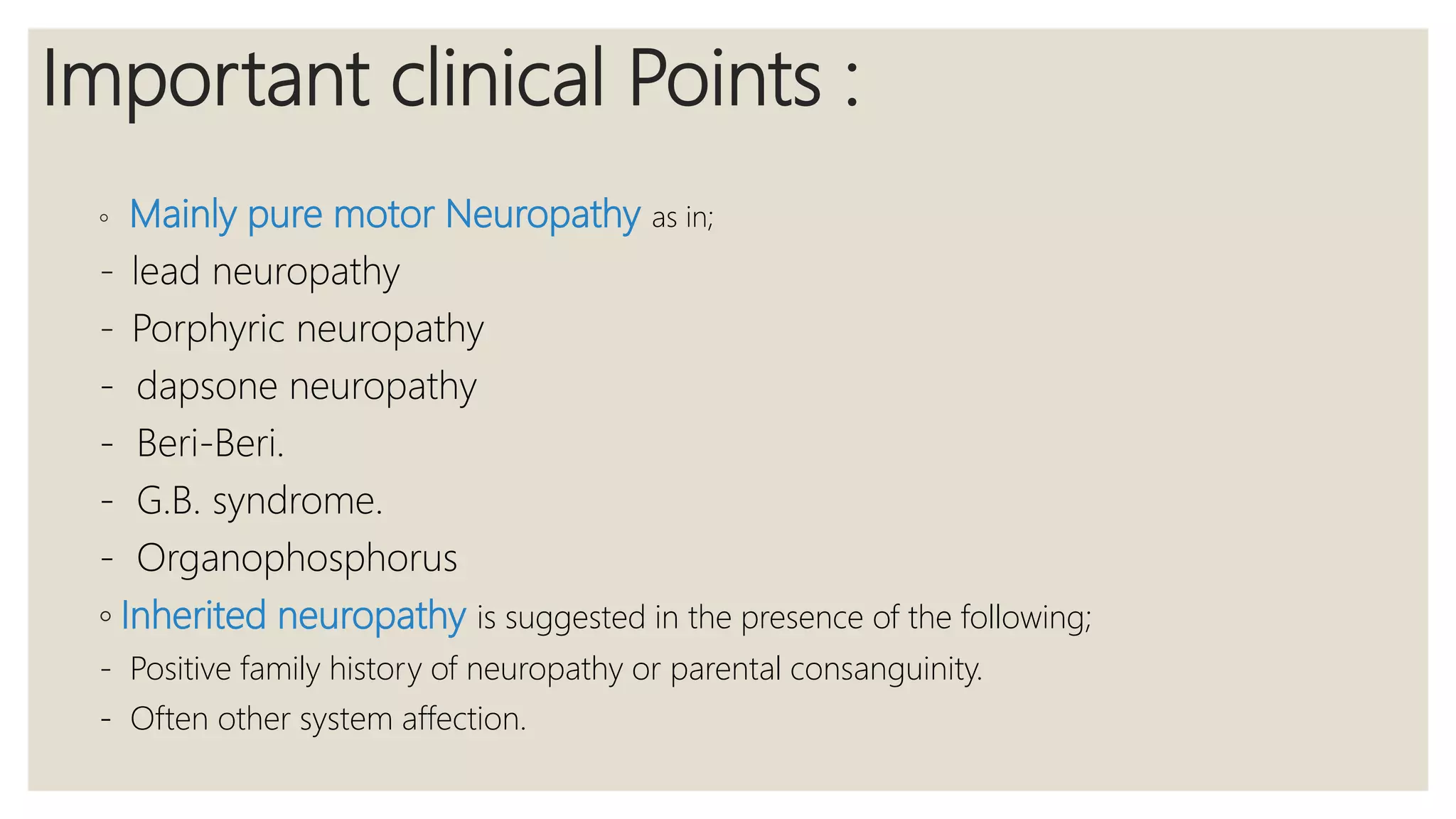
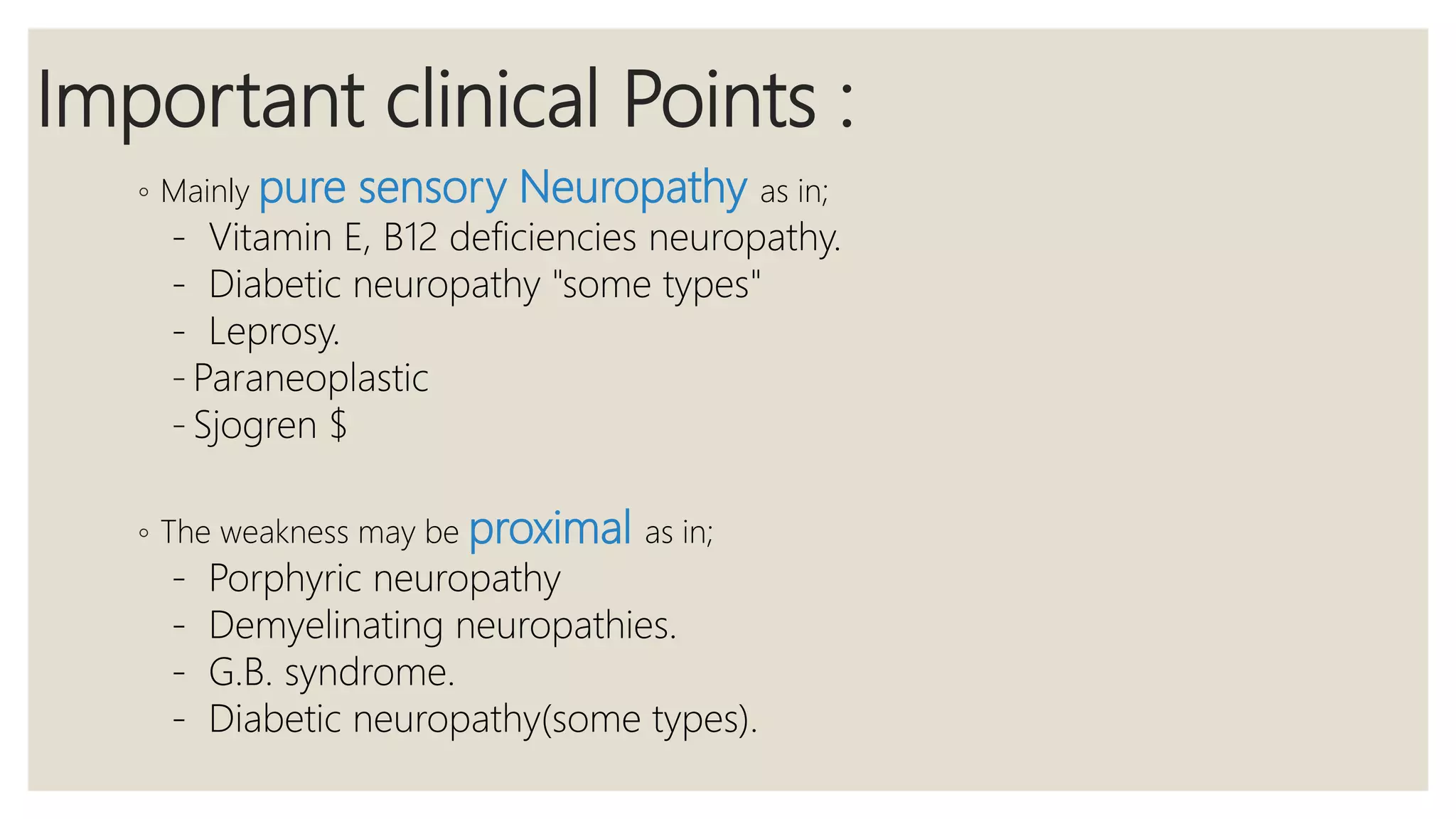
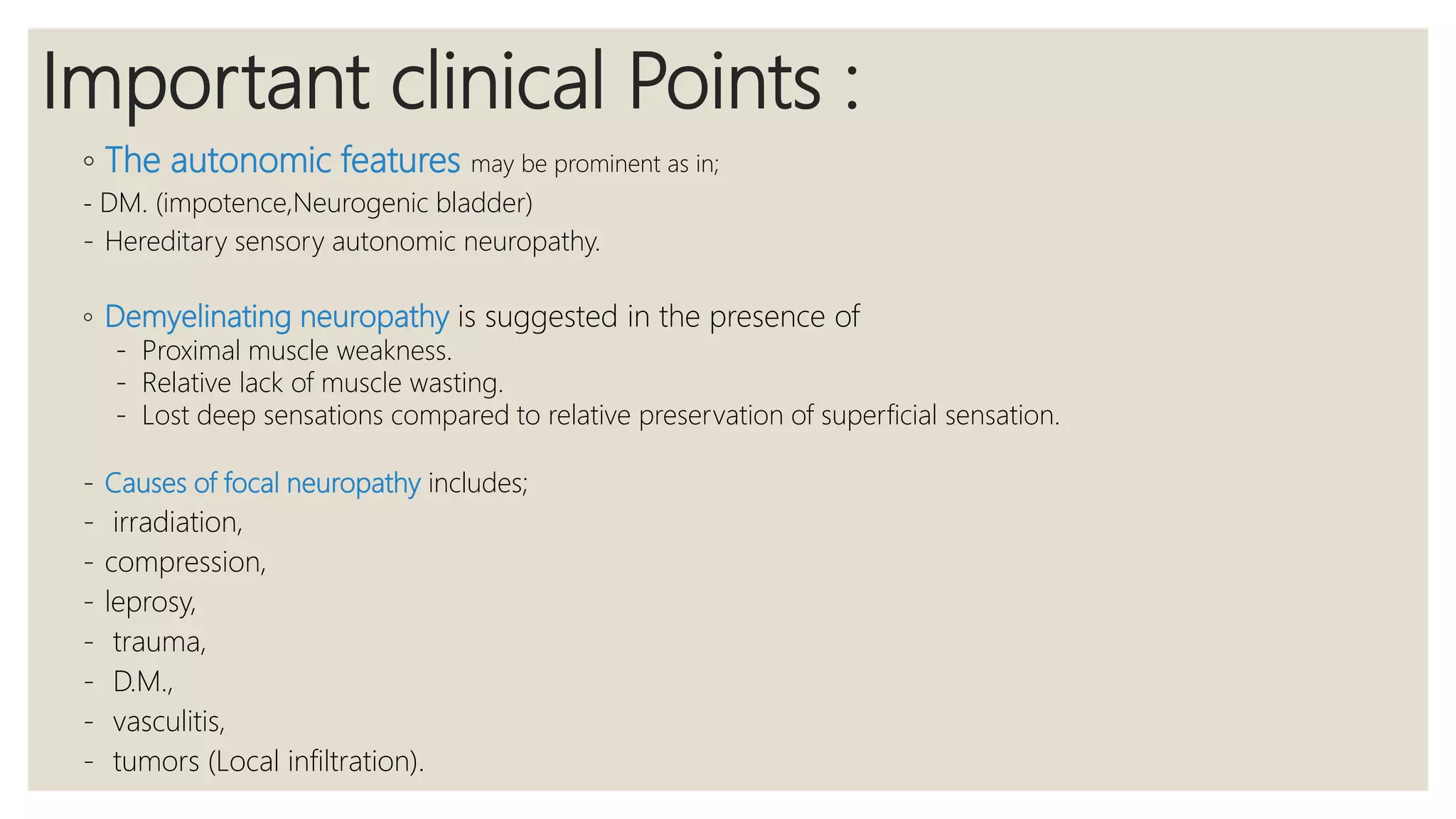
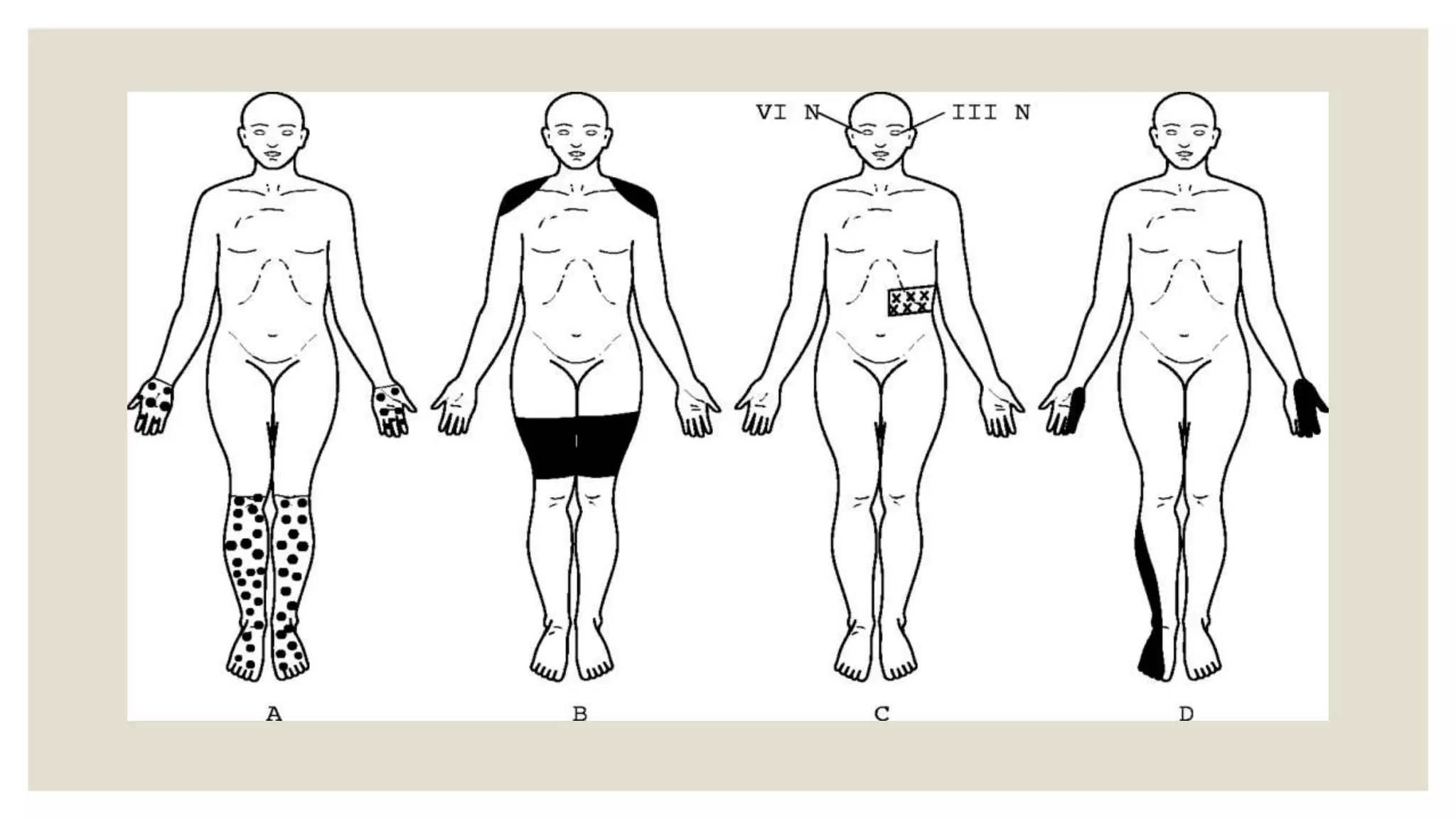
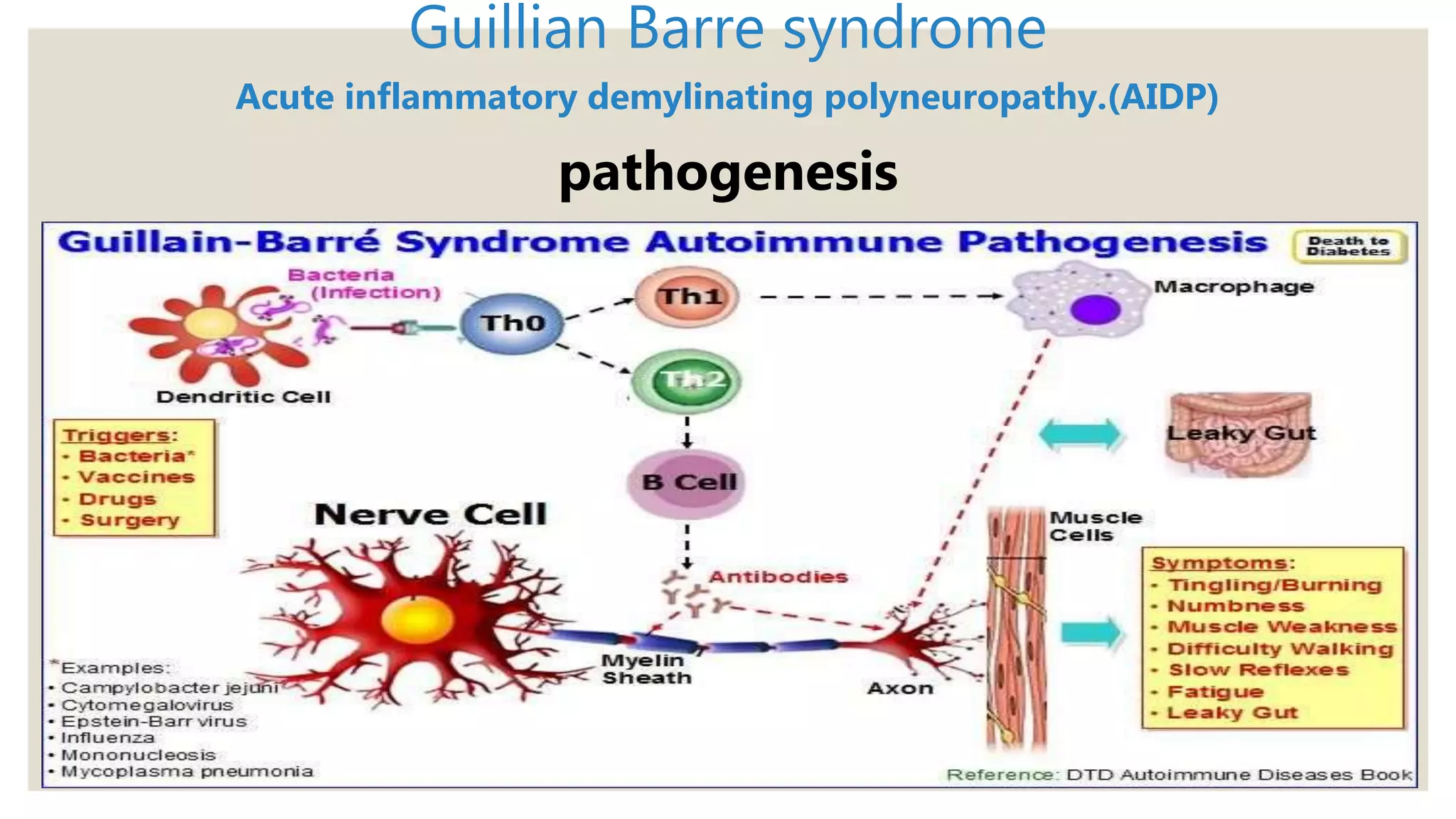
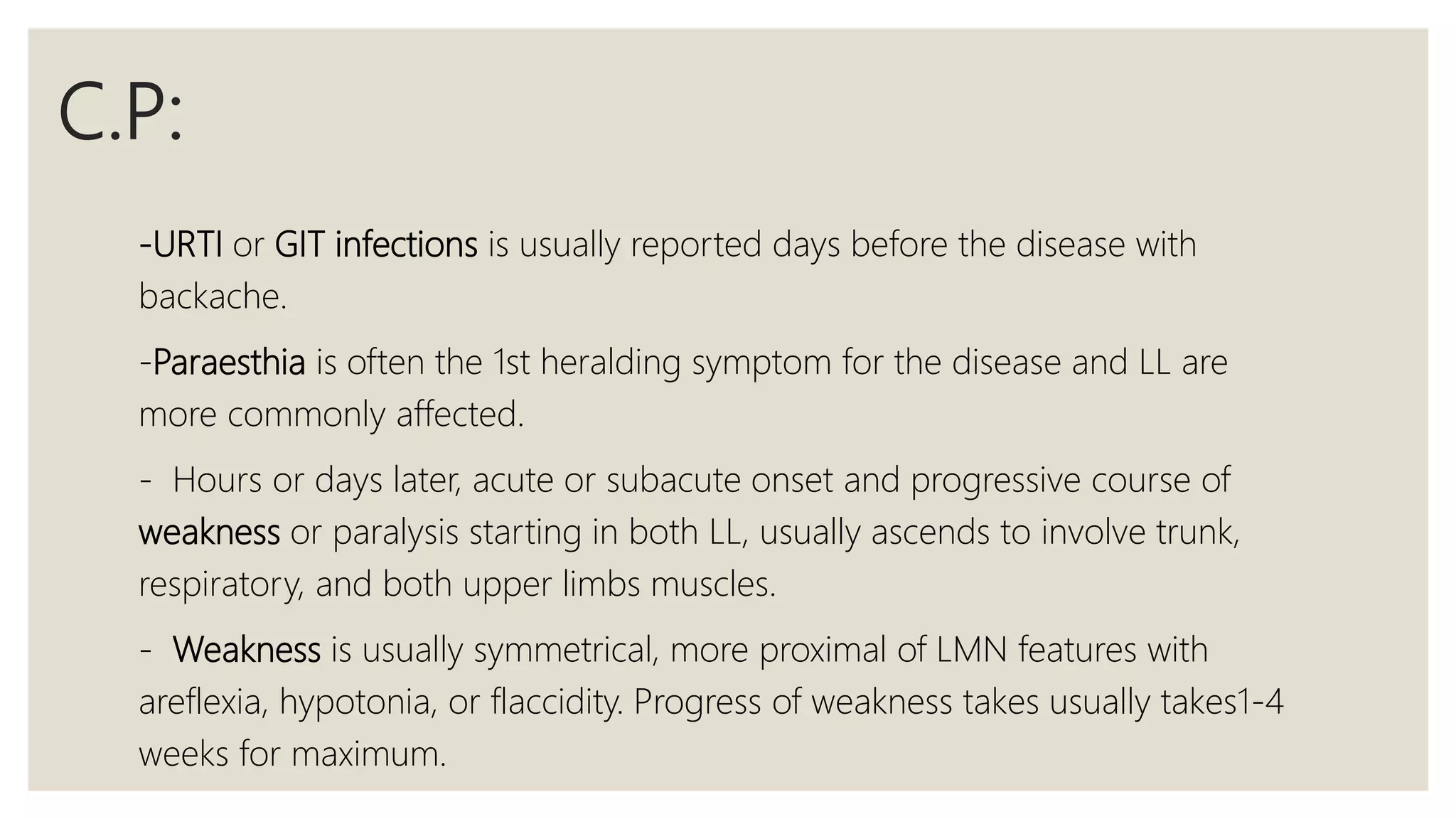
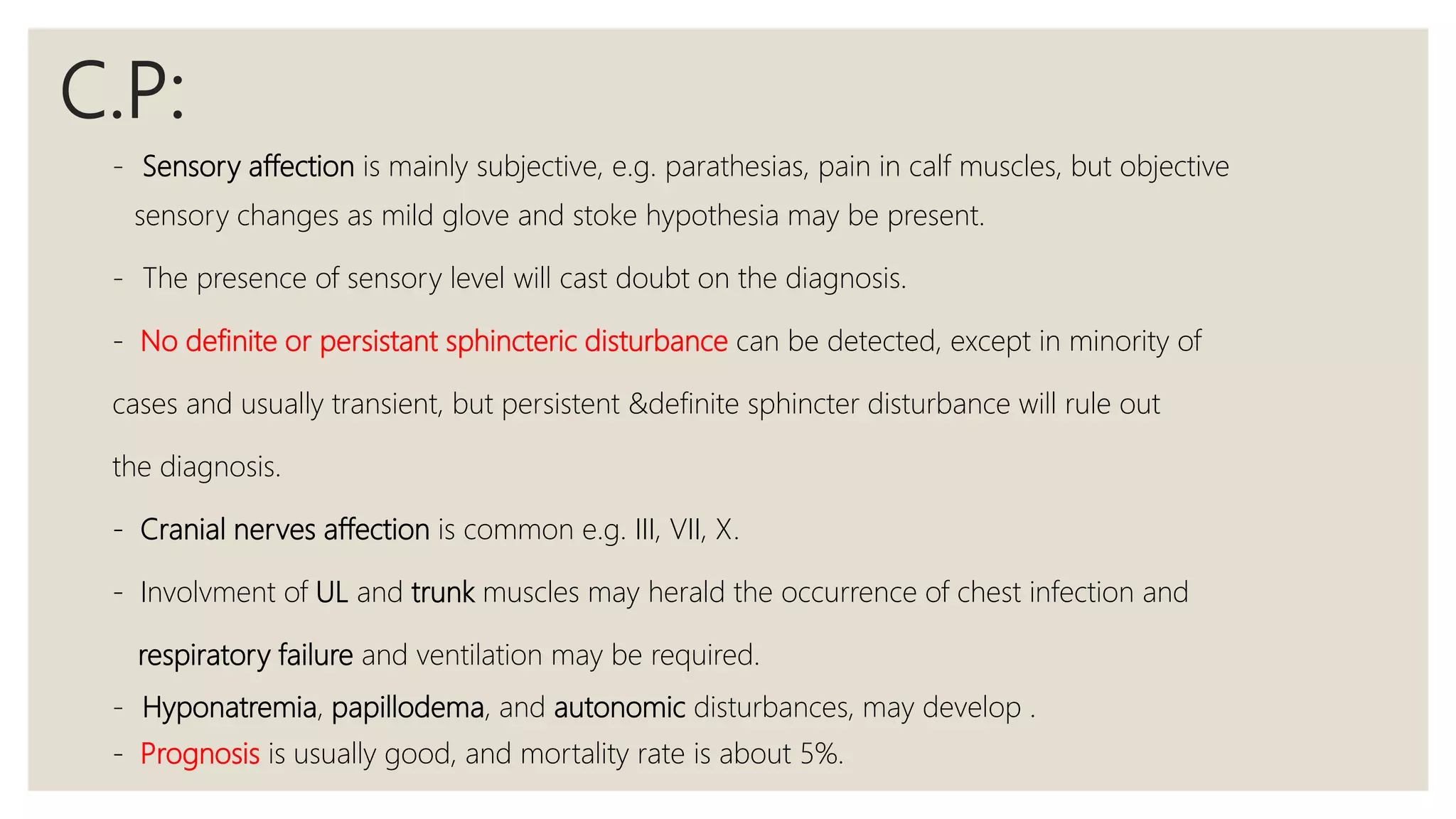
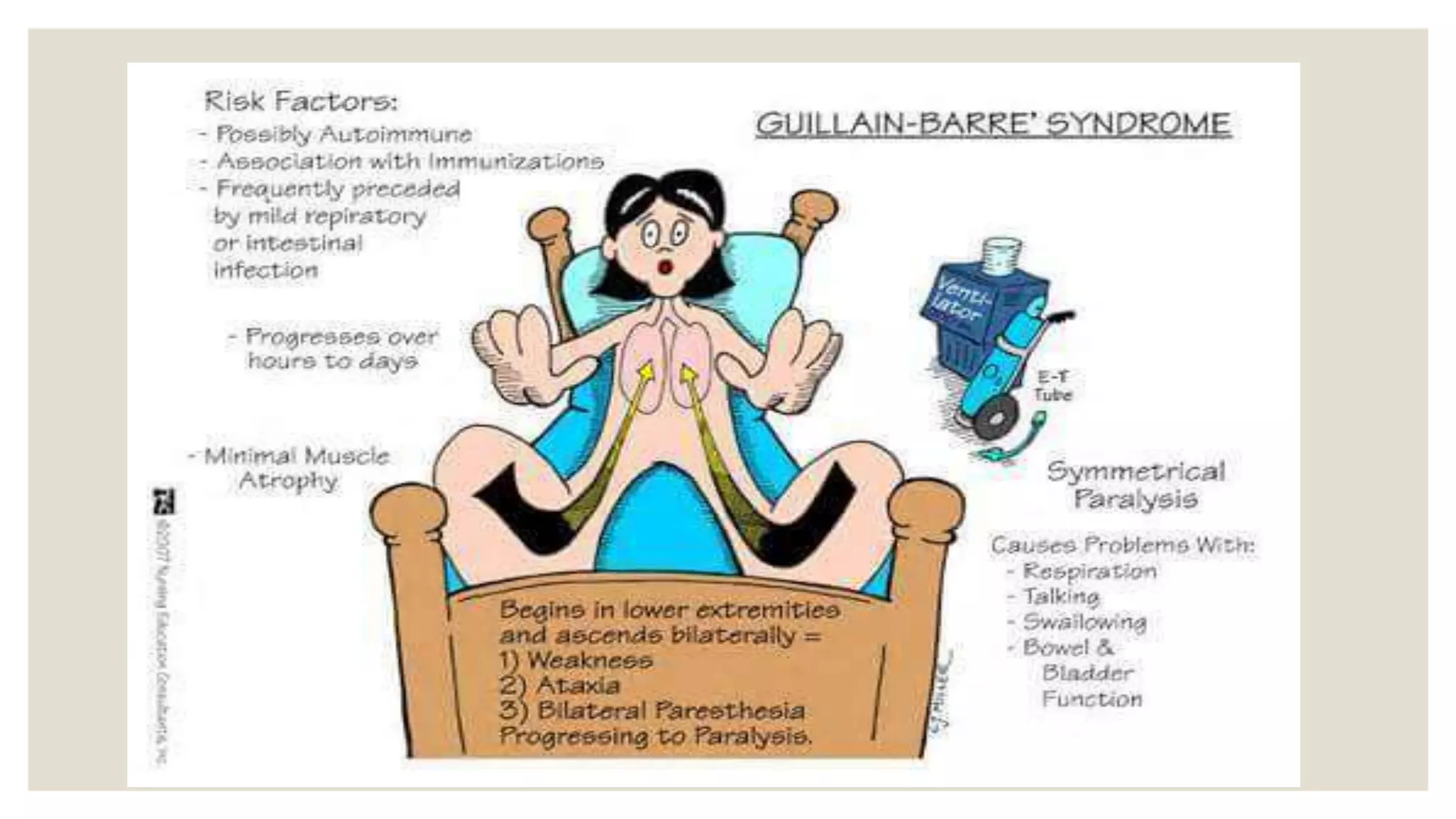
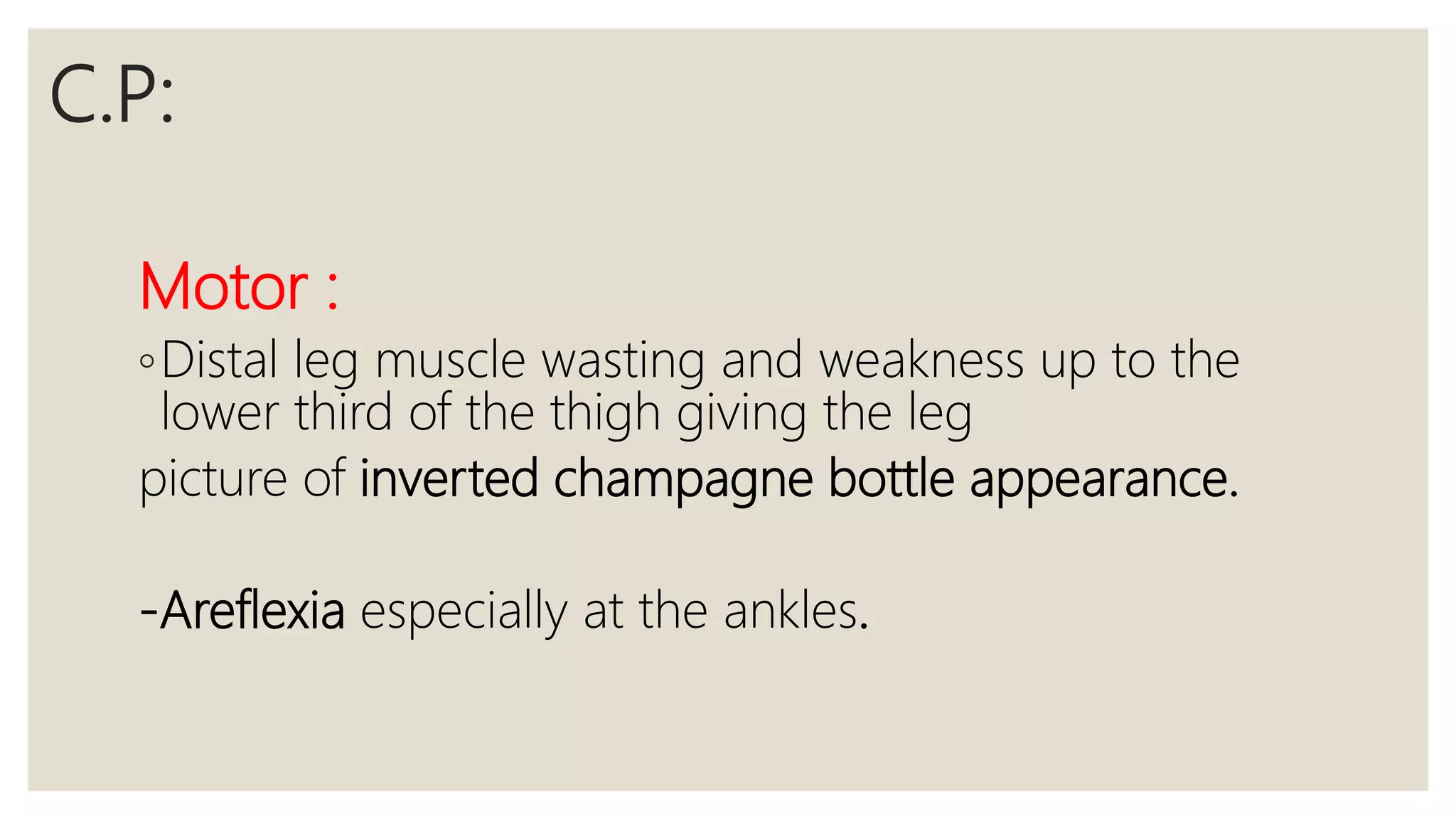
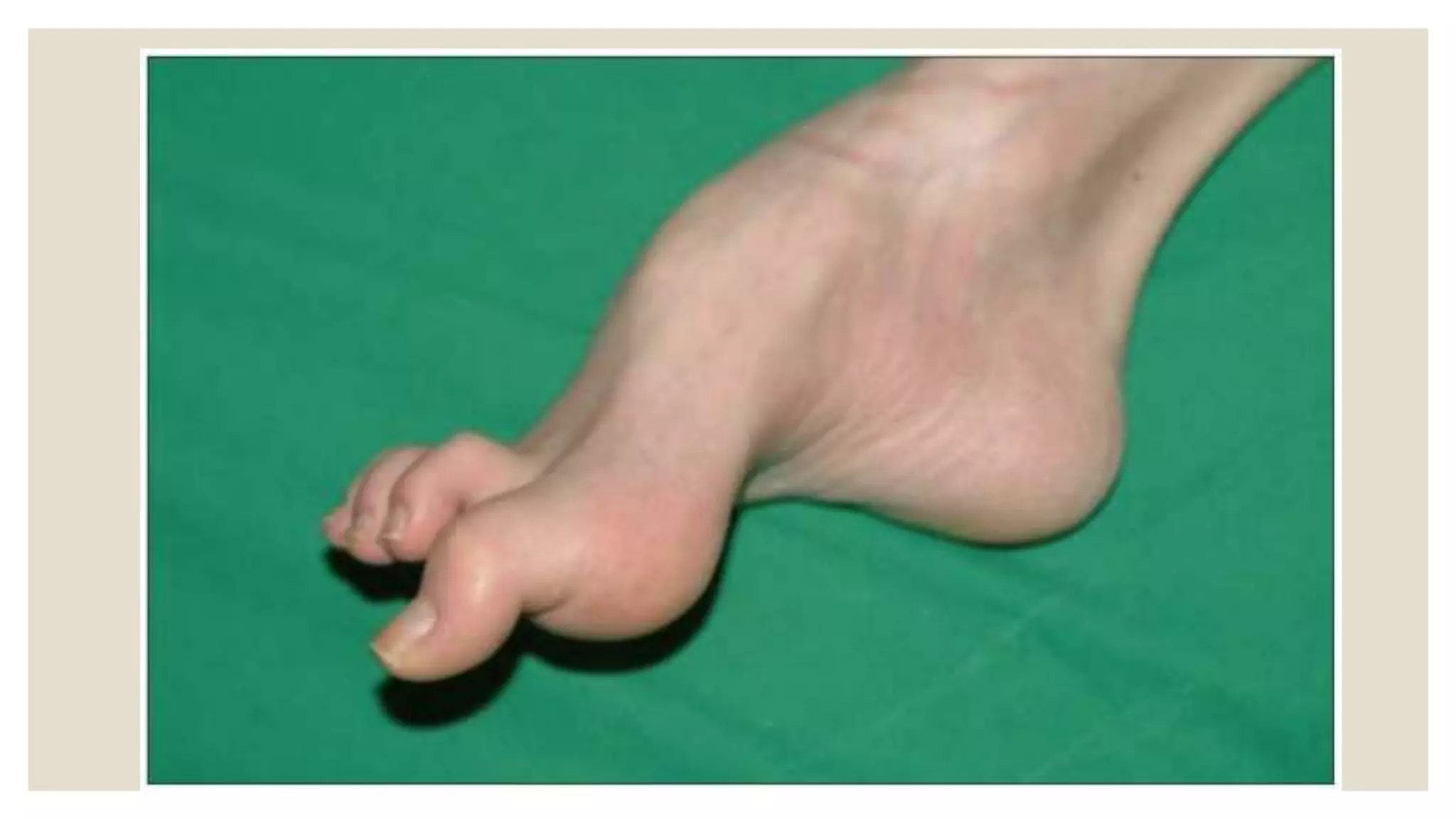
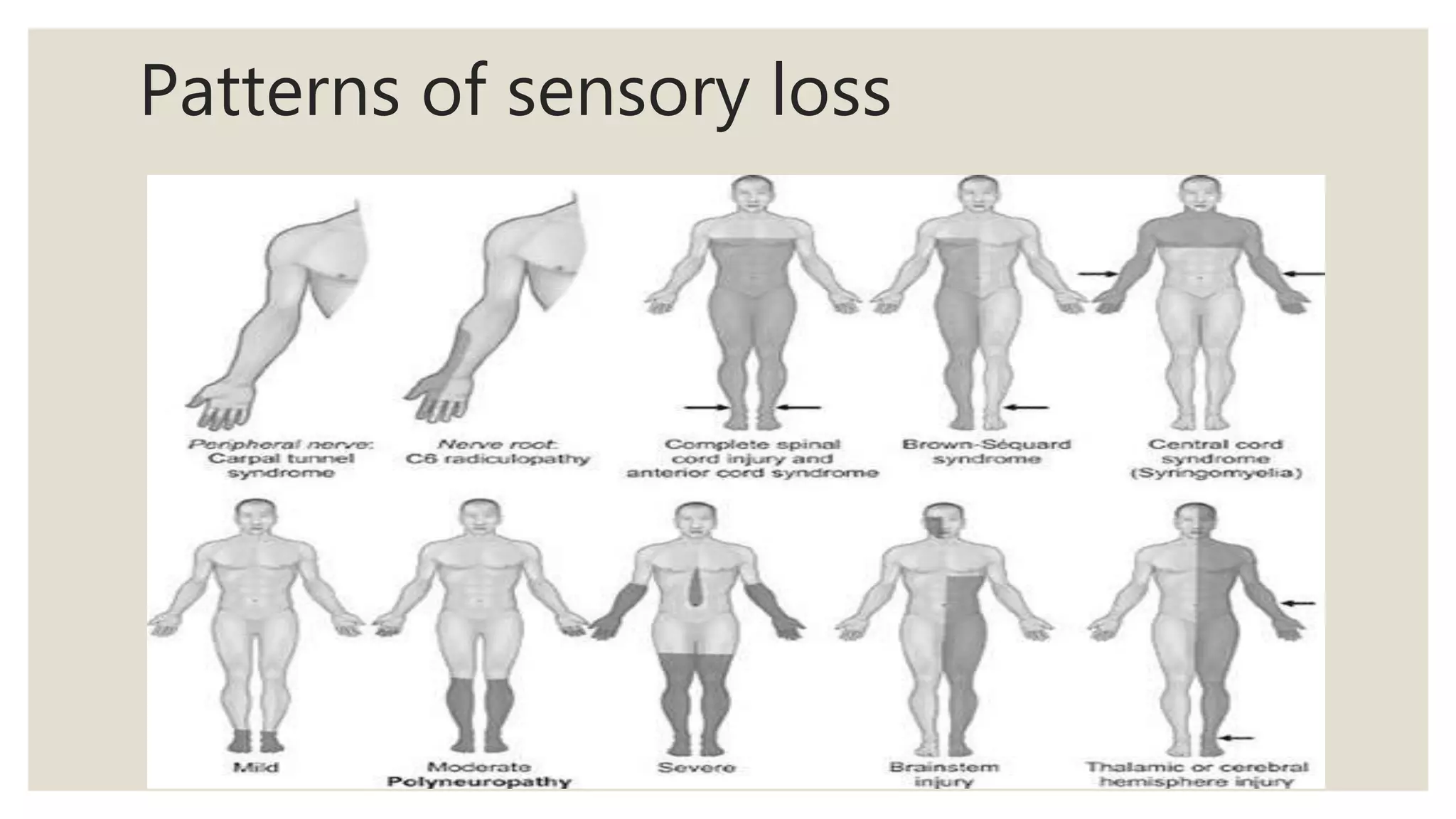
This document provides an overview of peripheral neuropathy. It defines peripheral neuropathy as inflammation or degeneration of peripheral nerves or cranial nerves leading to motor and/or sensory dysfunction. It then classifies peripheral neuropathies and discusses various causes including inherited, acquired, infectious, toxic and metabolic. Clinical features, investigations and management are described for different types of peripheral neuropathy such as diabetic neuropathy, Guillain-Barre syndrome and Charcot-Marie-Tooth disease. Key examination findings and the presentations of different neuropathies are highlighted.