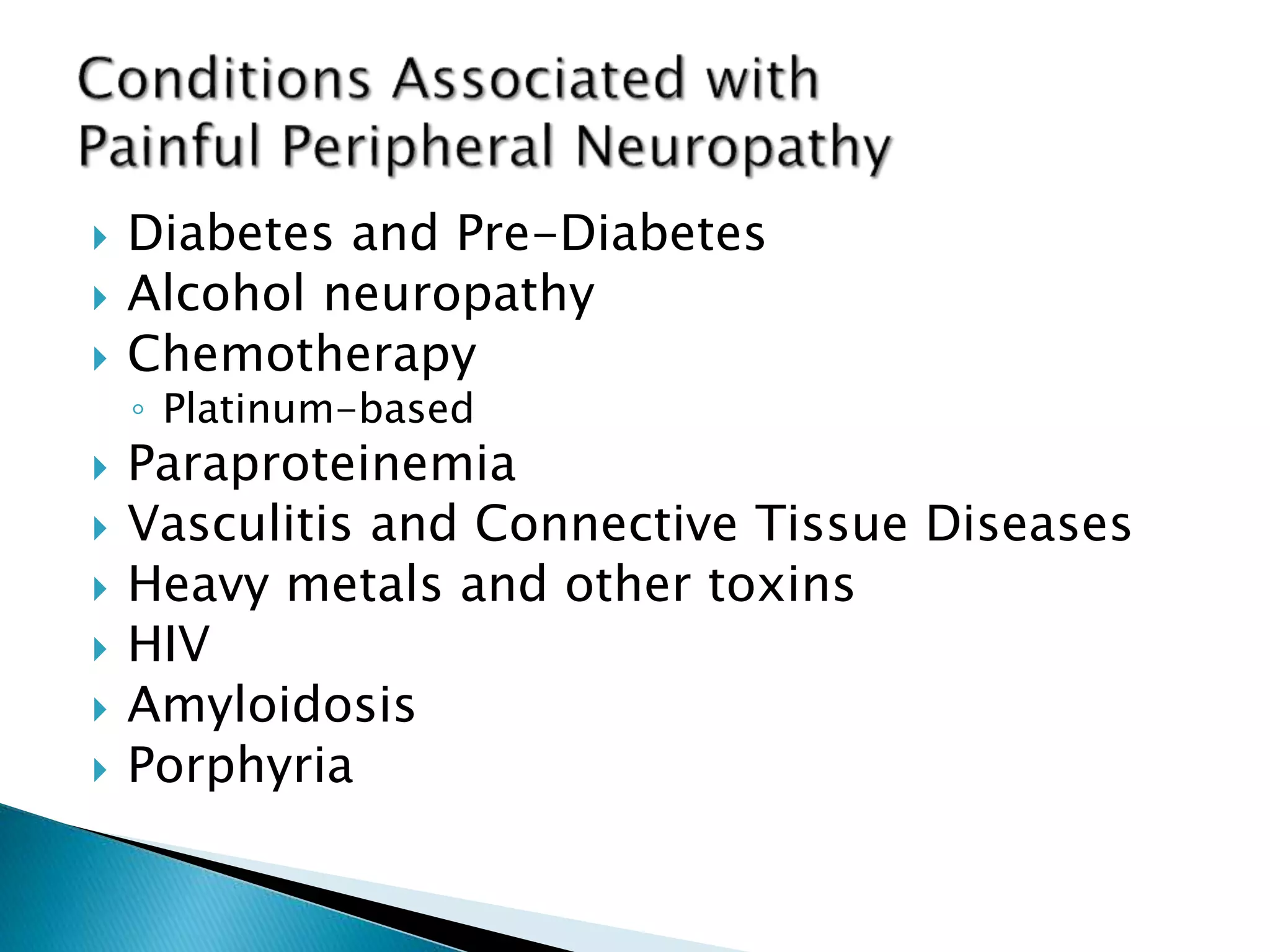
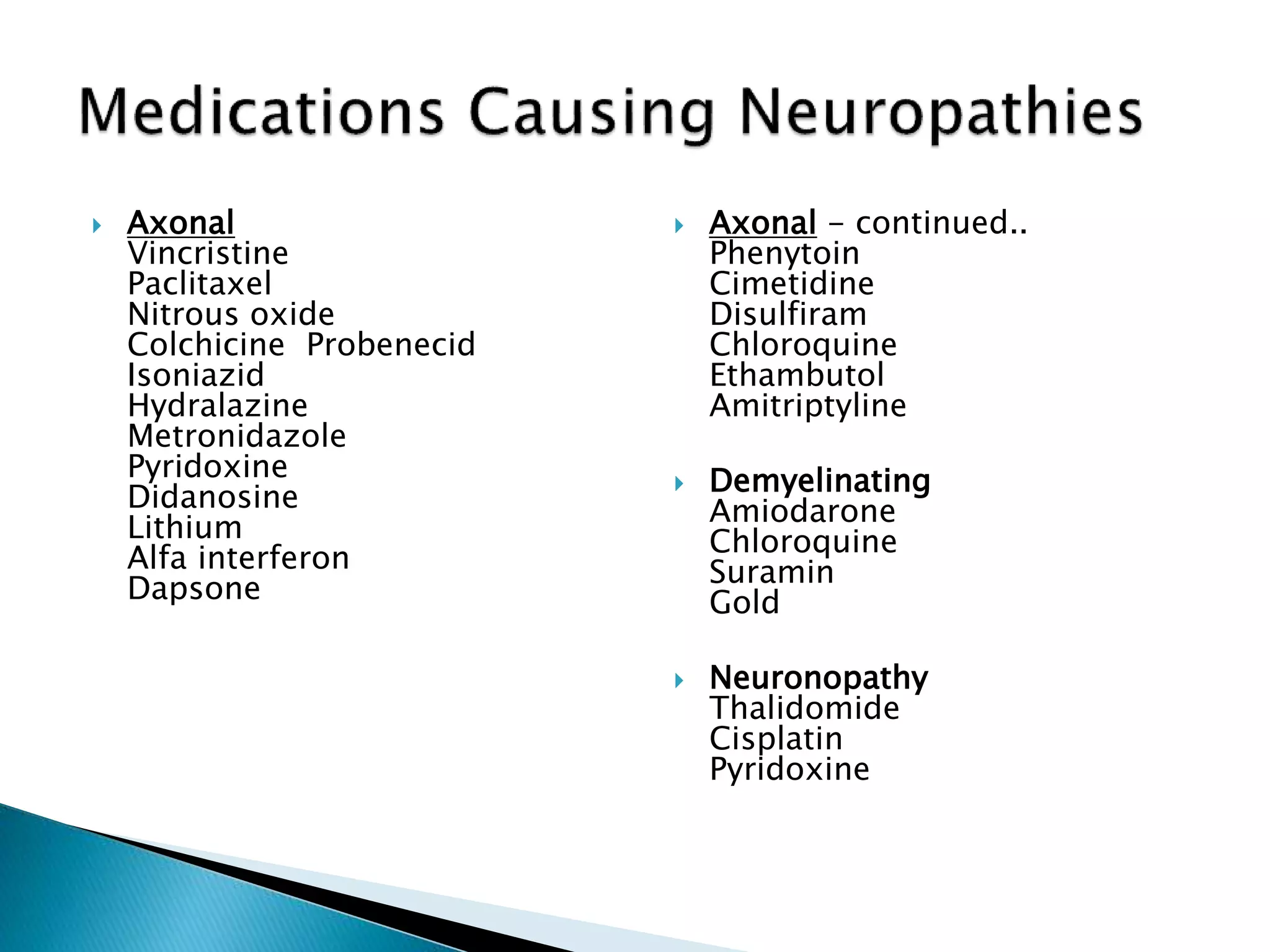
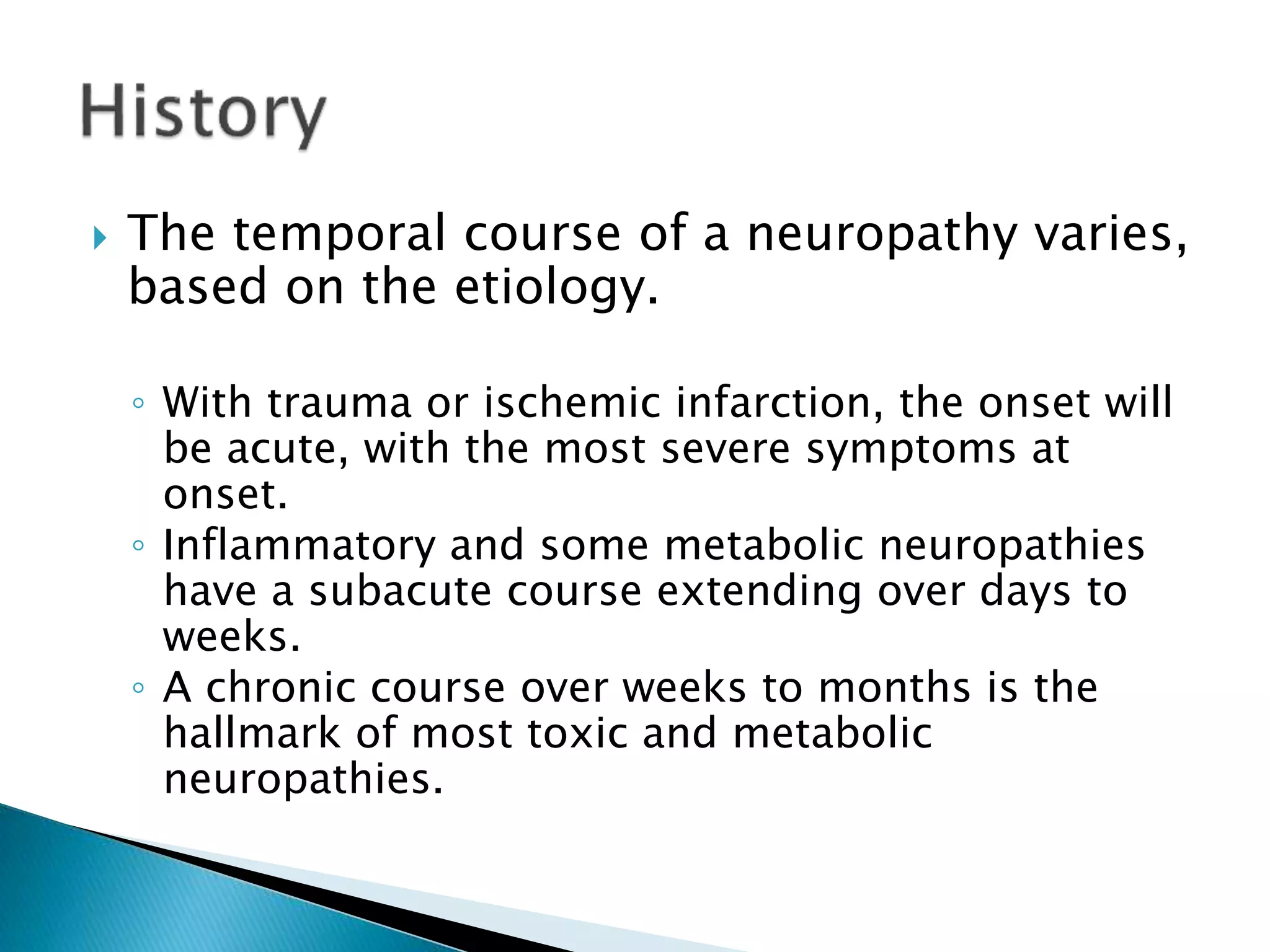
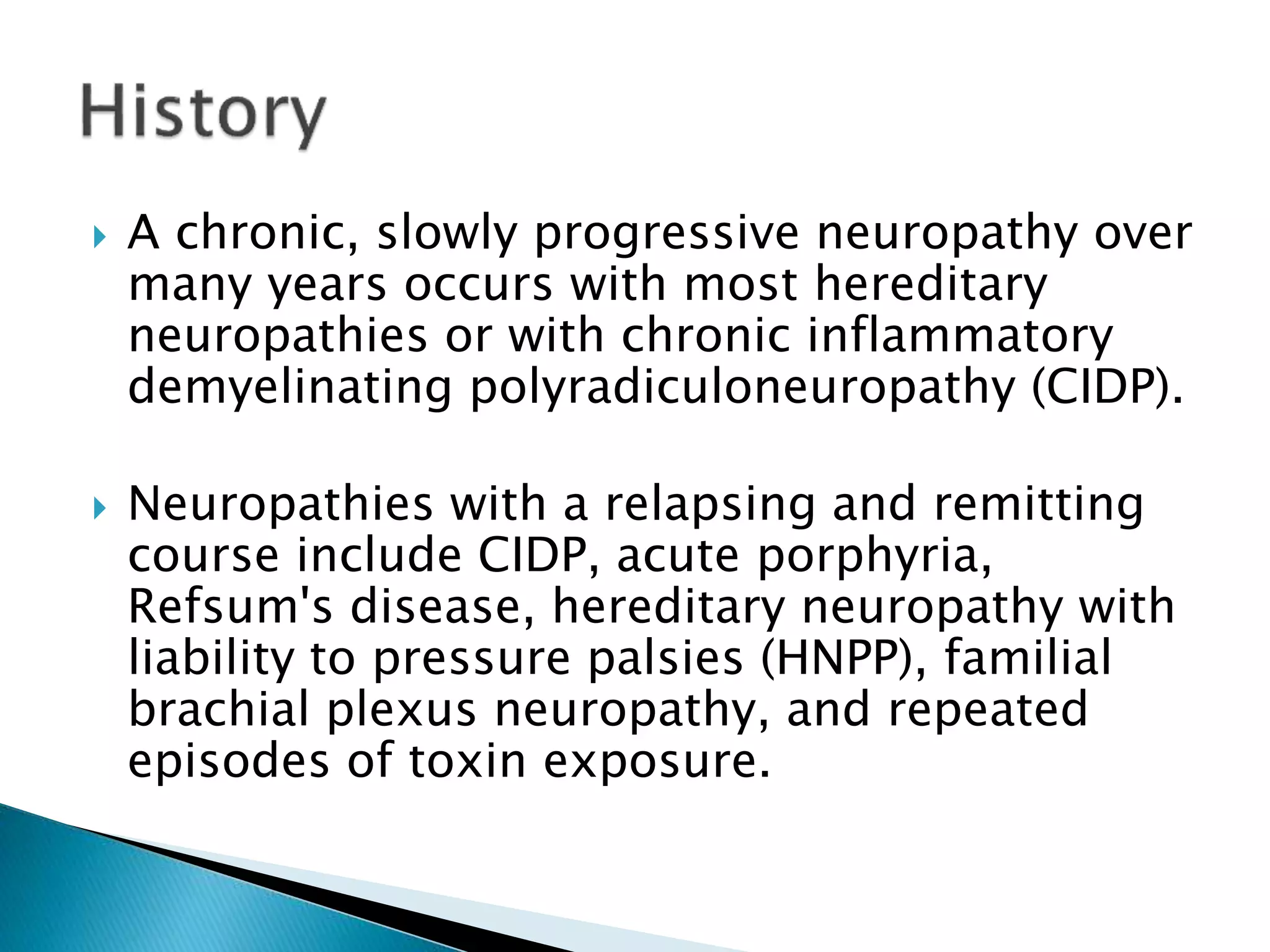
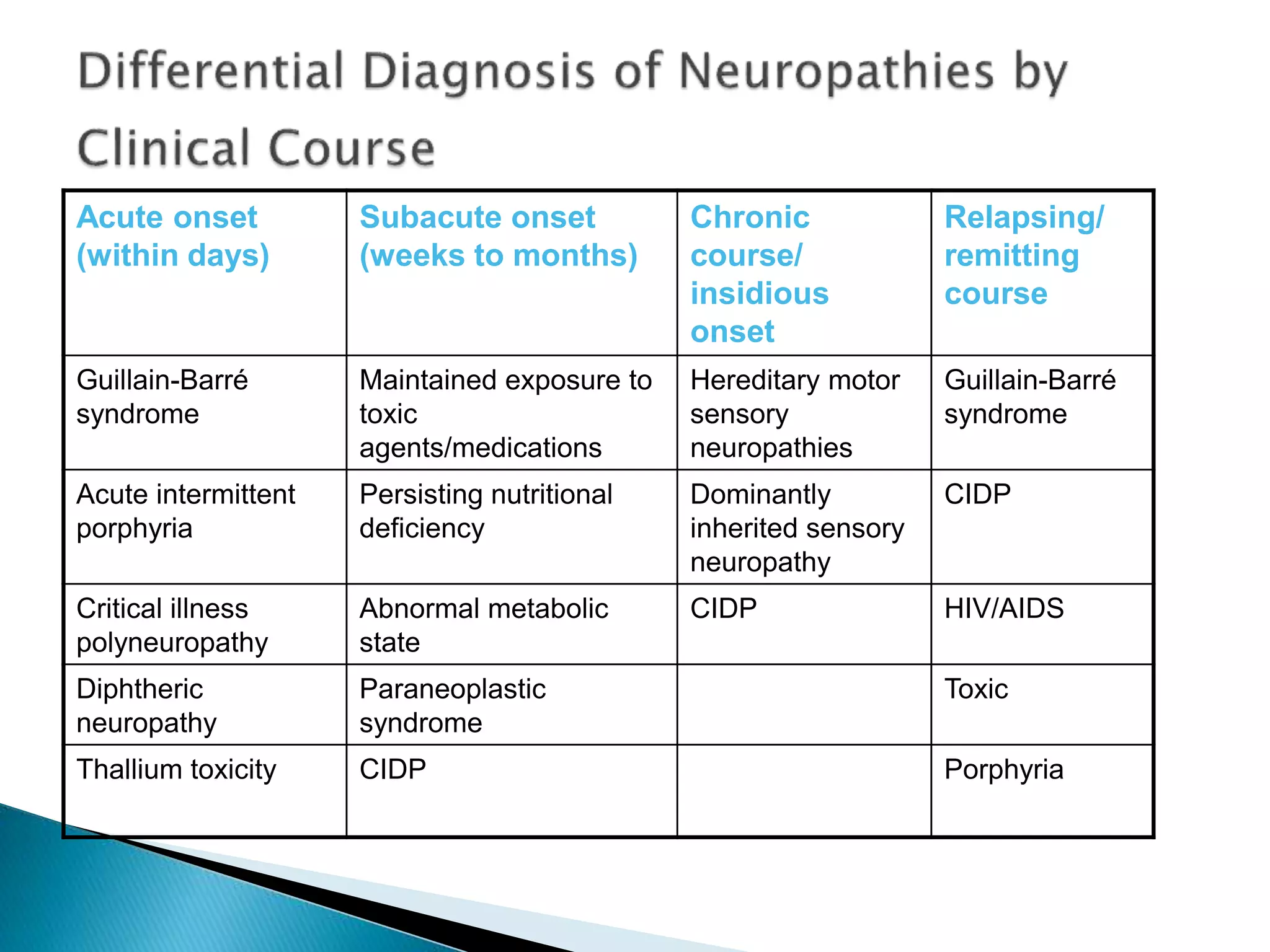
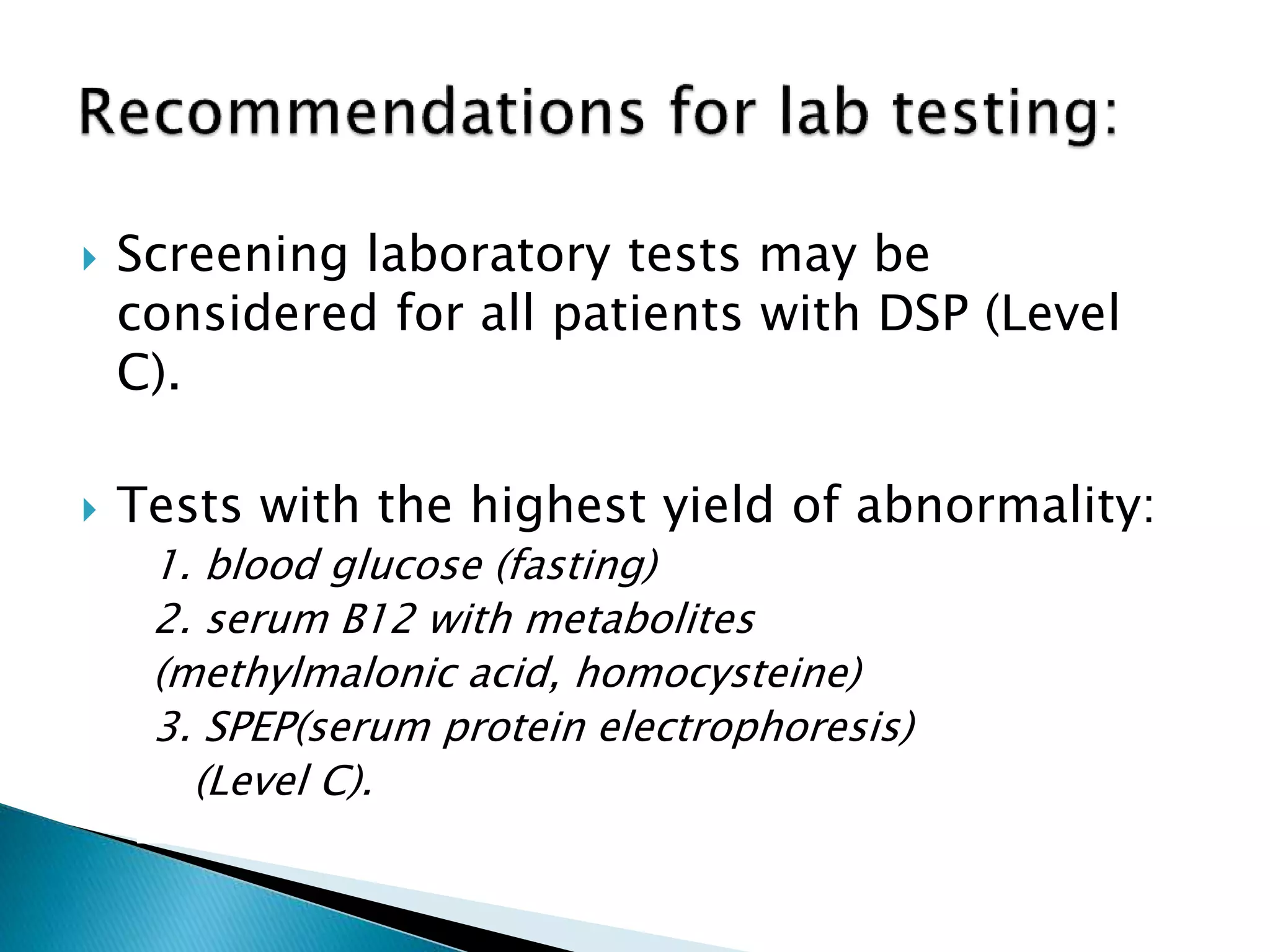
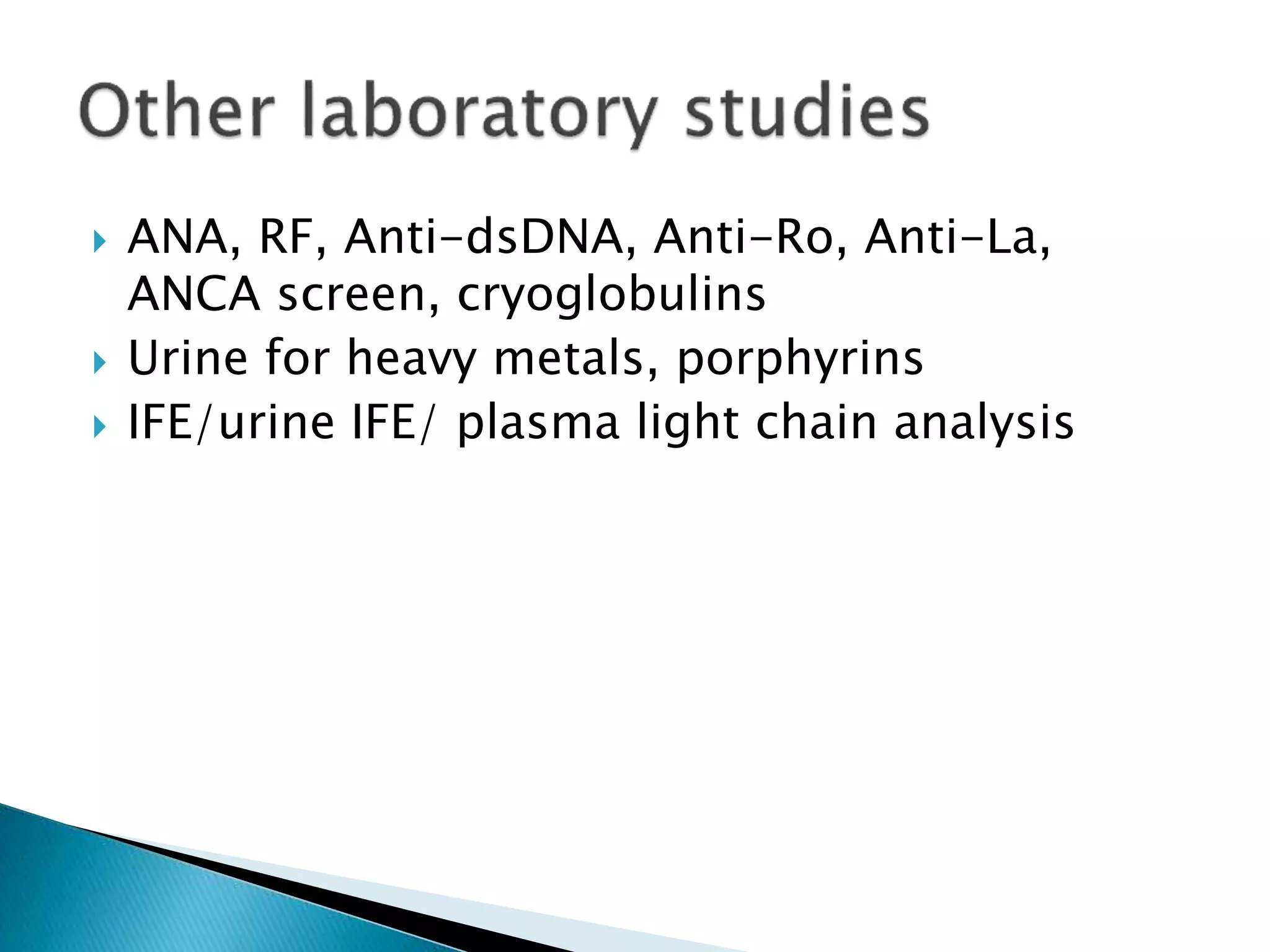
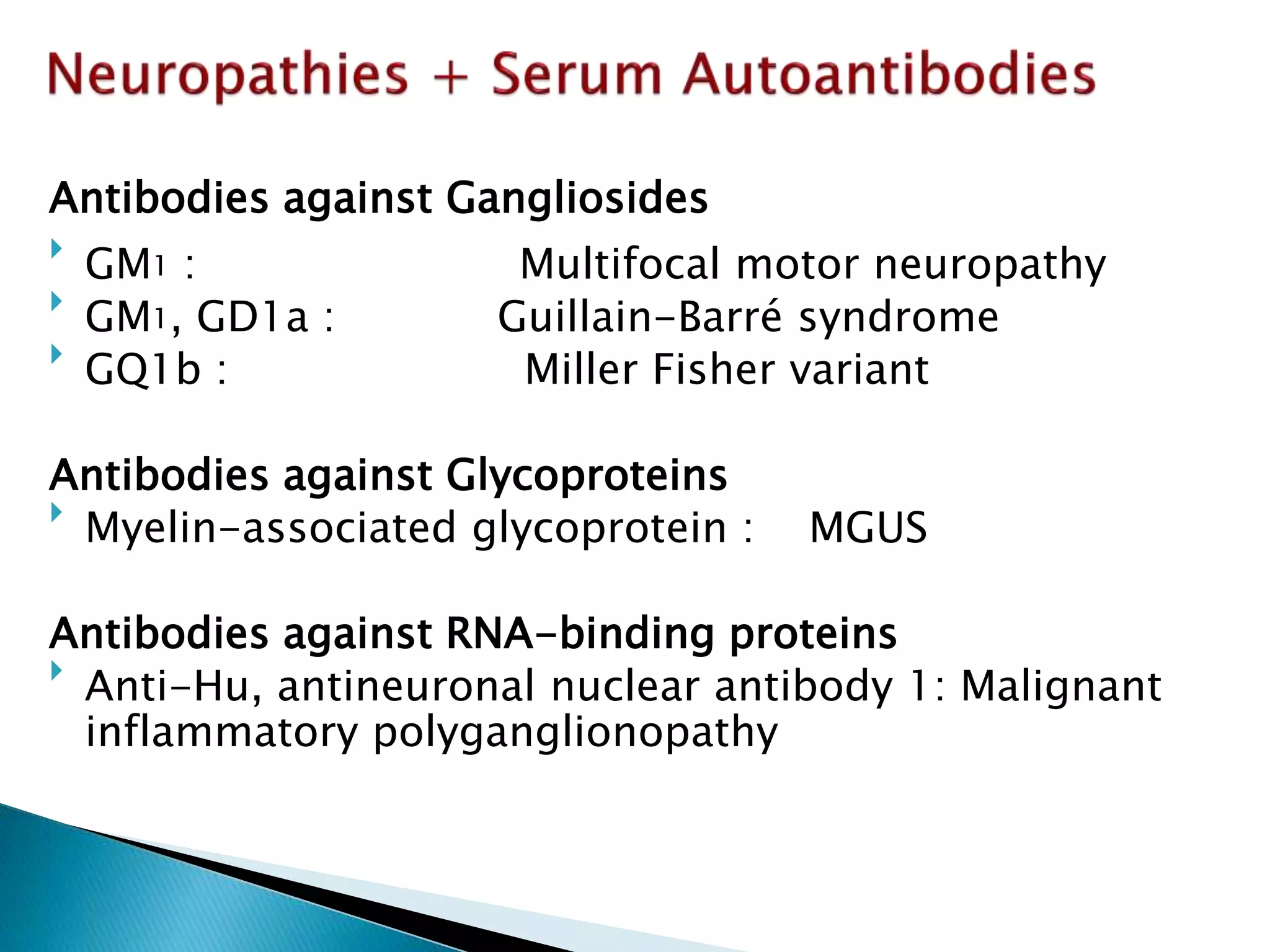
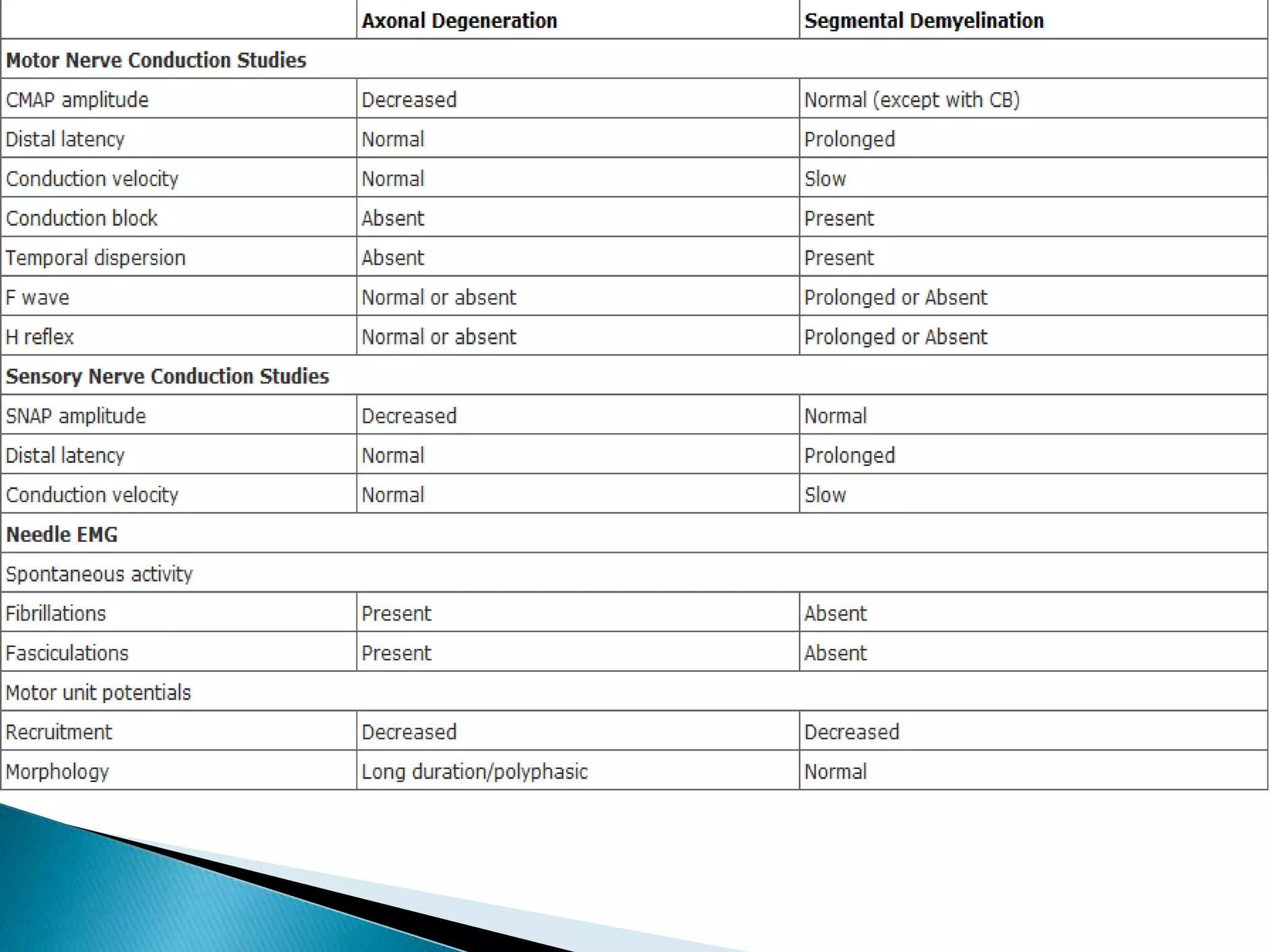
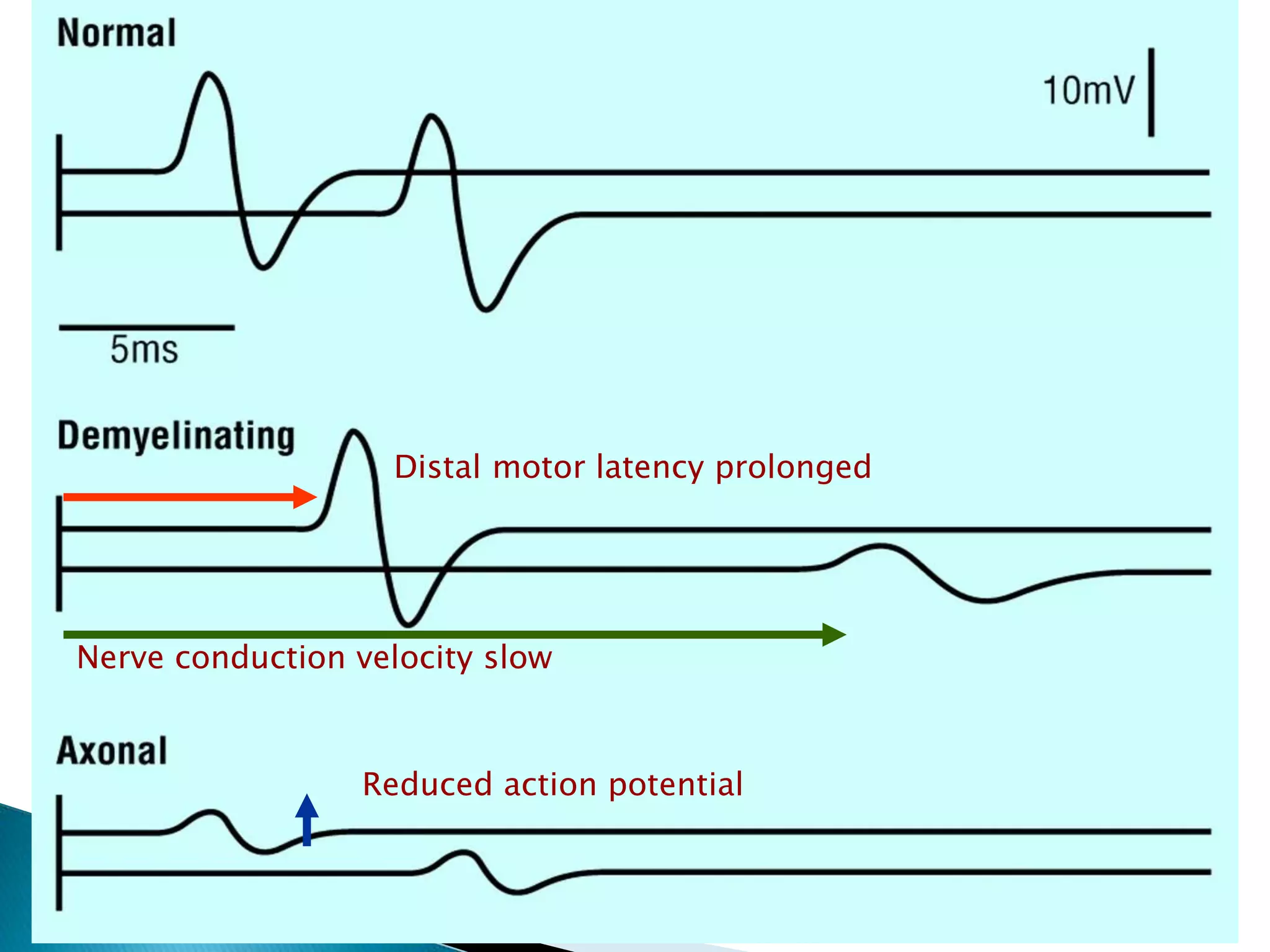
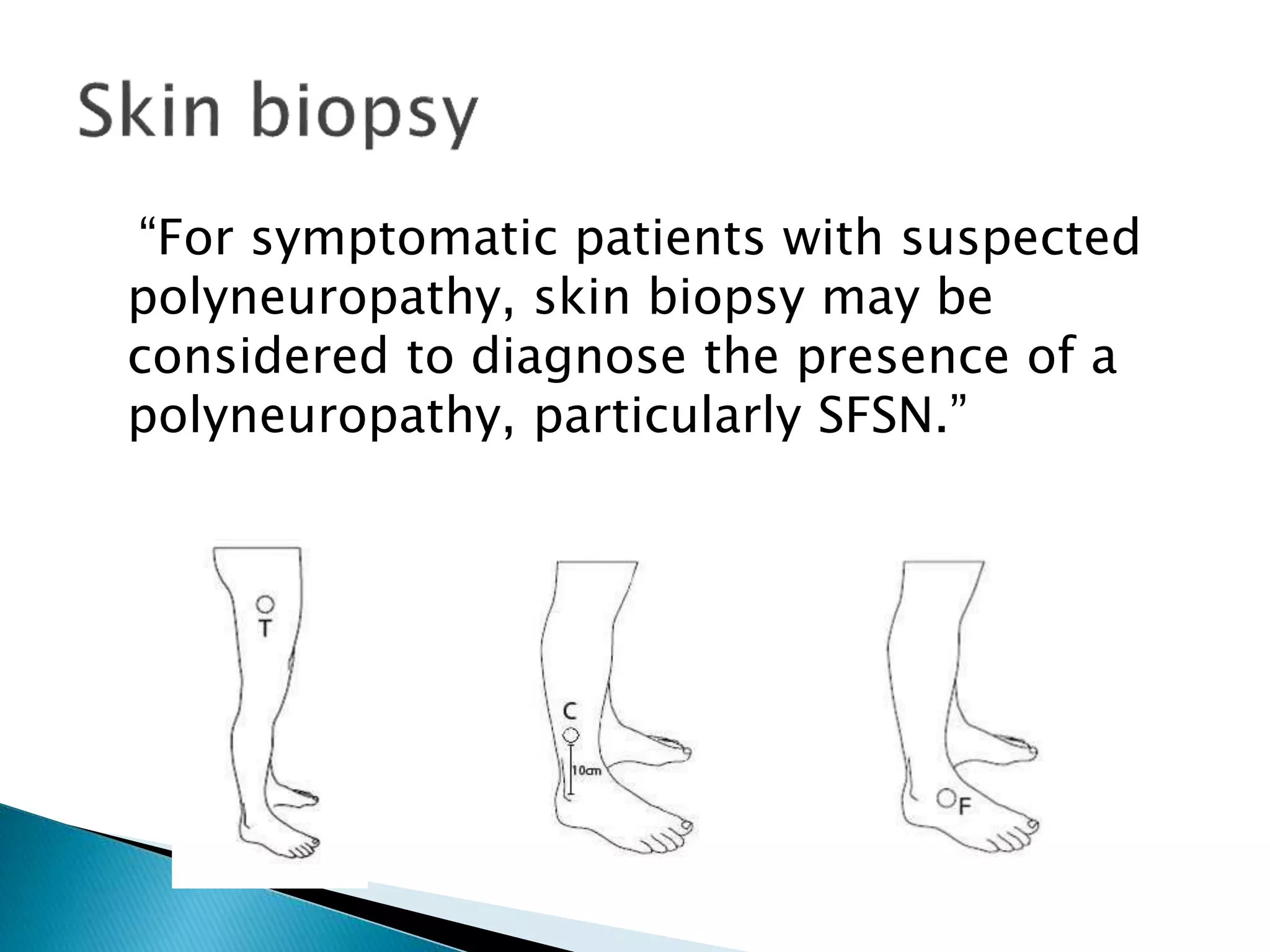
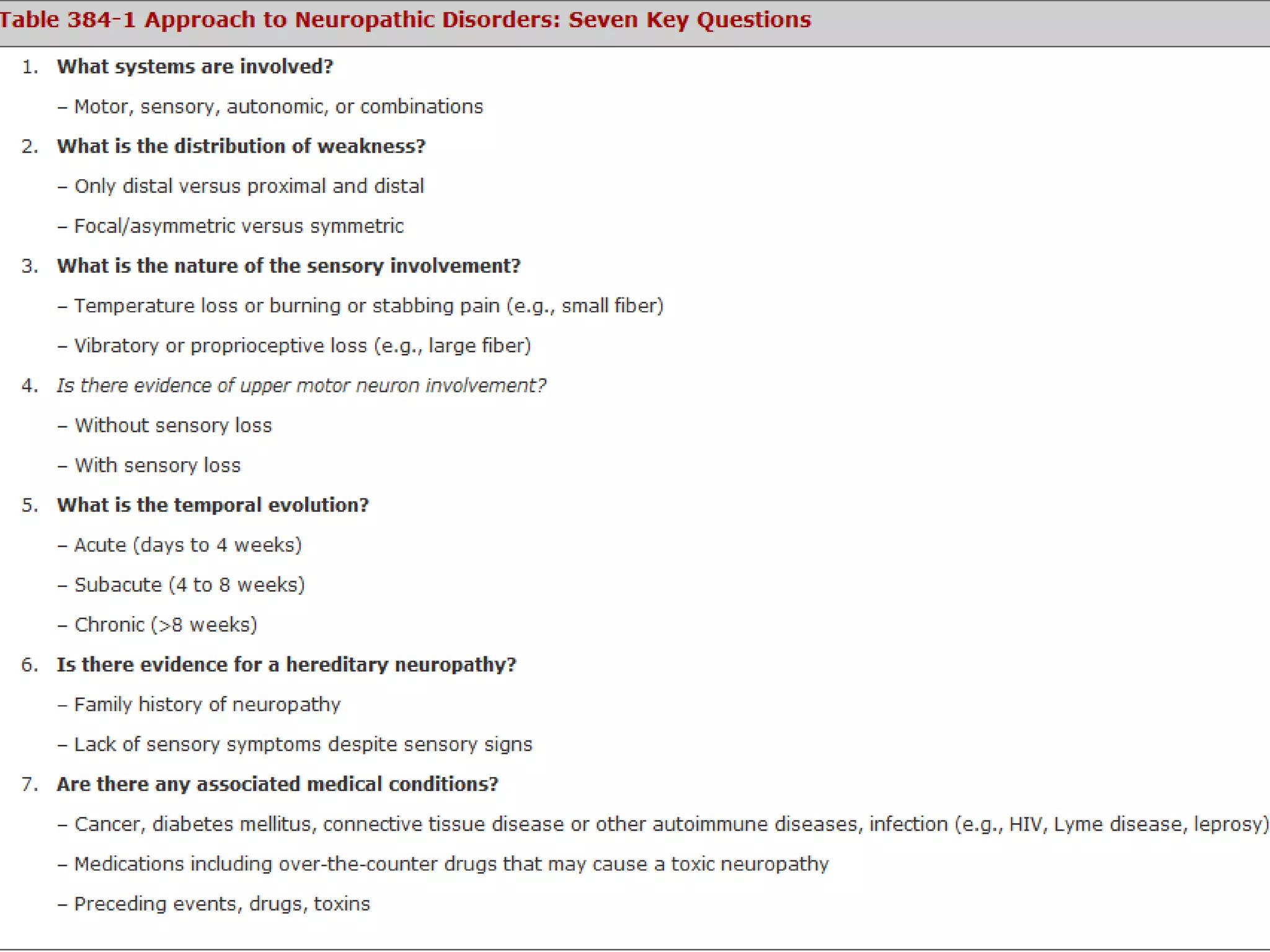
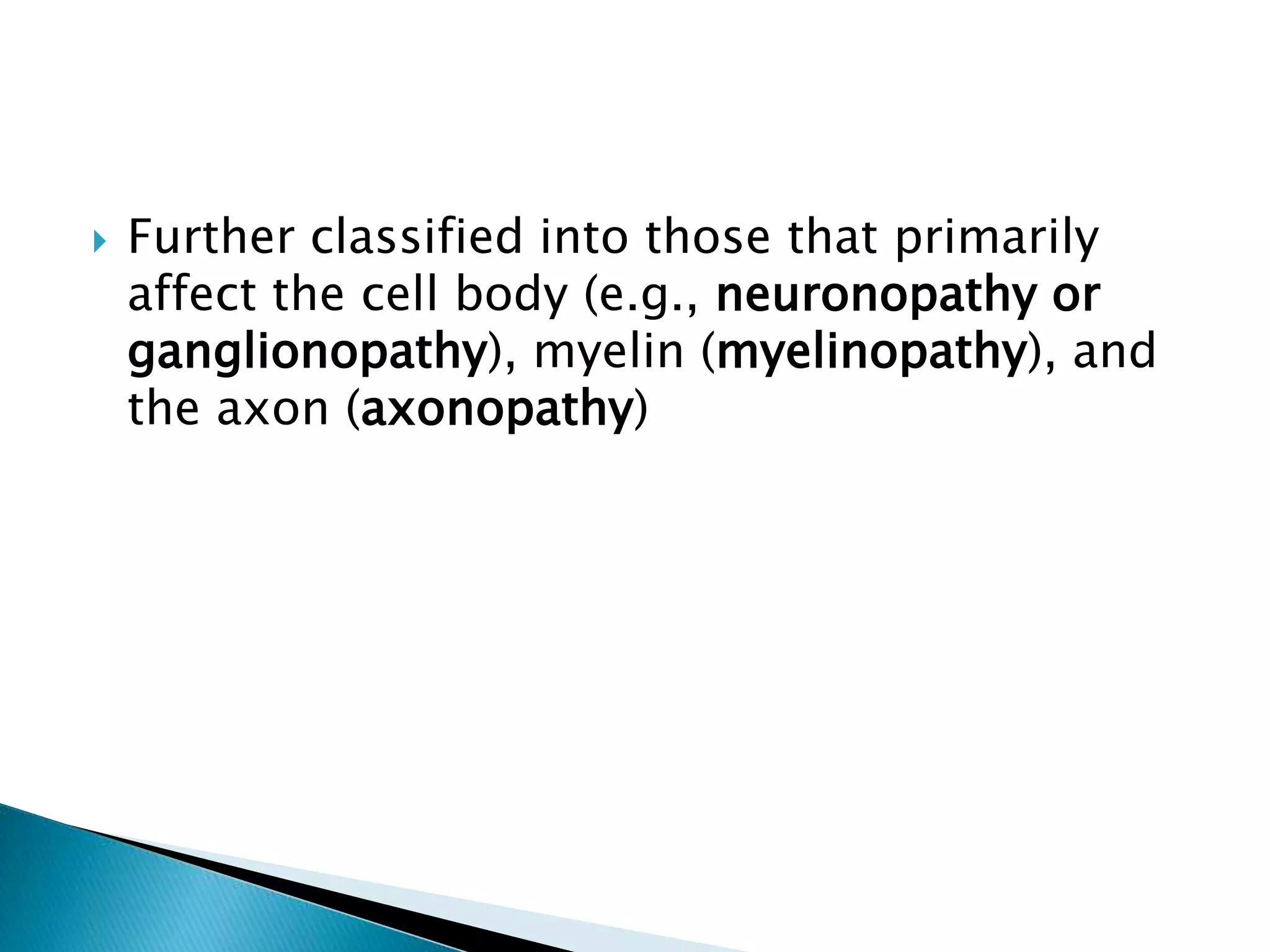
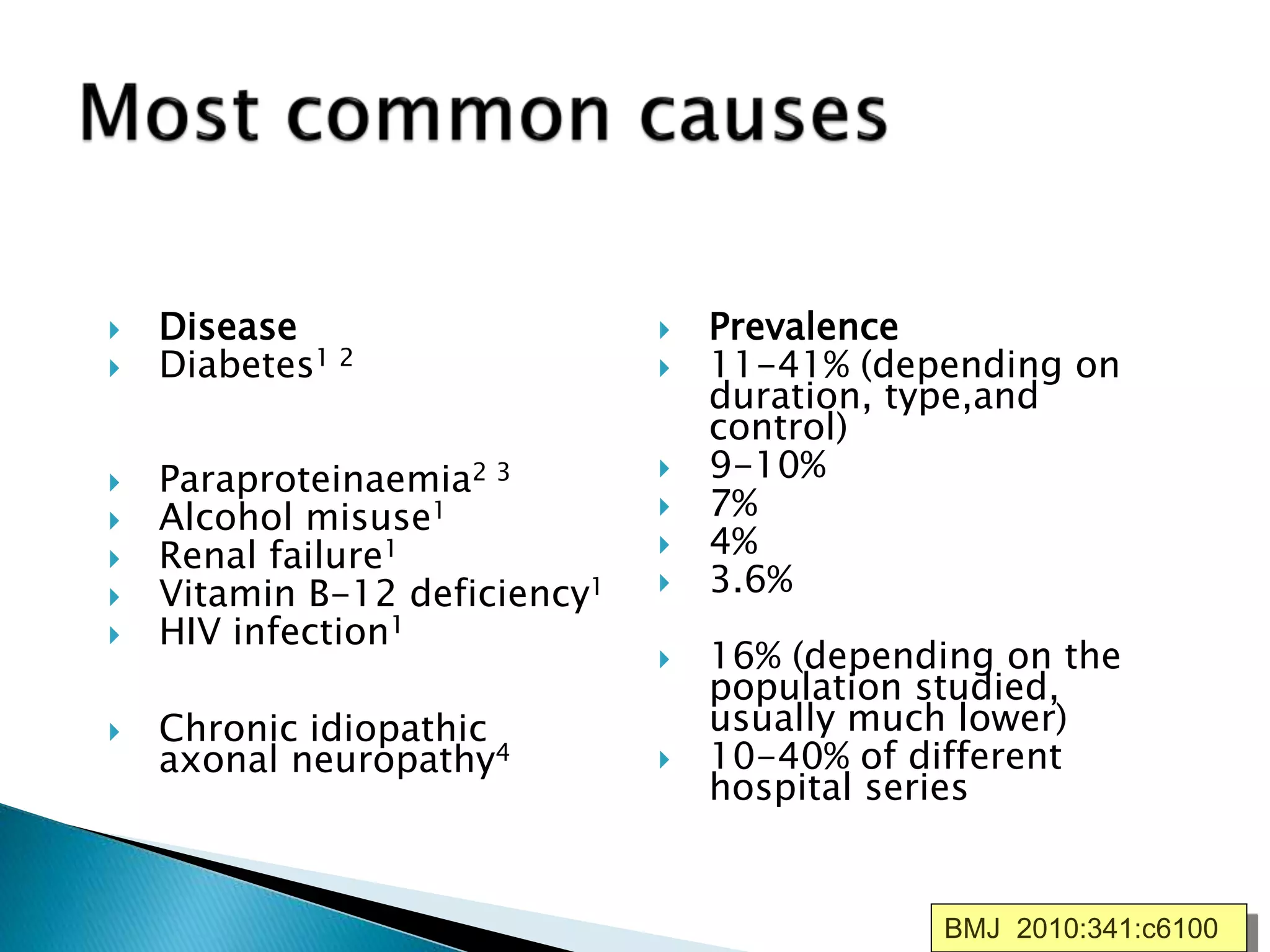
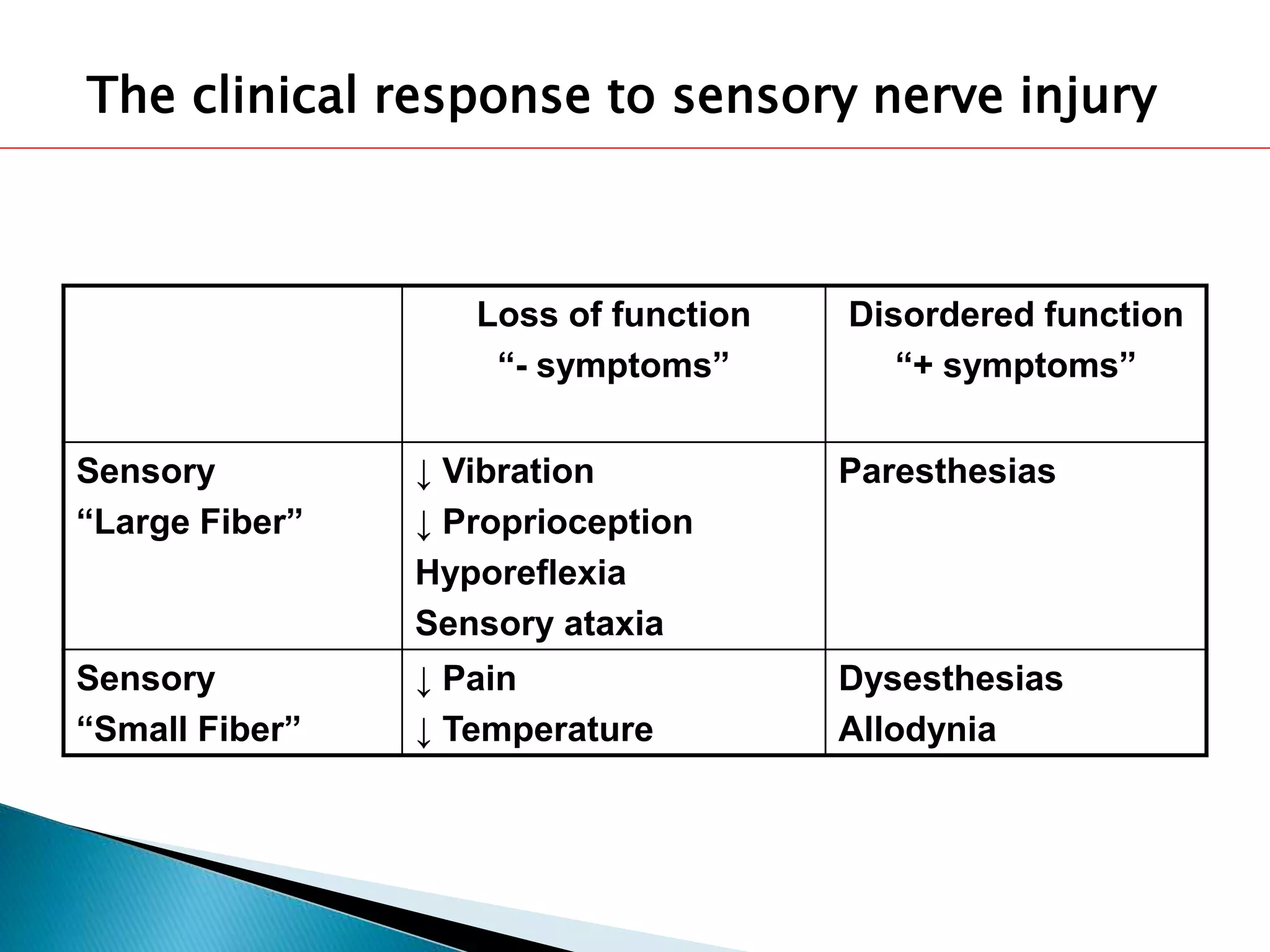
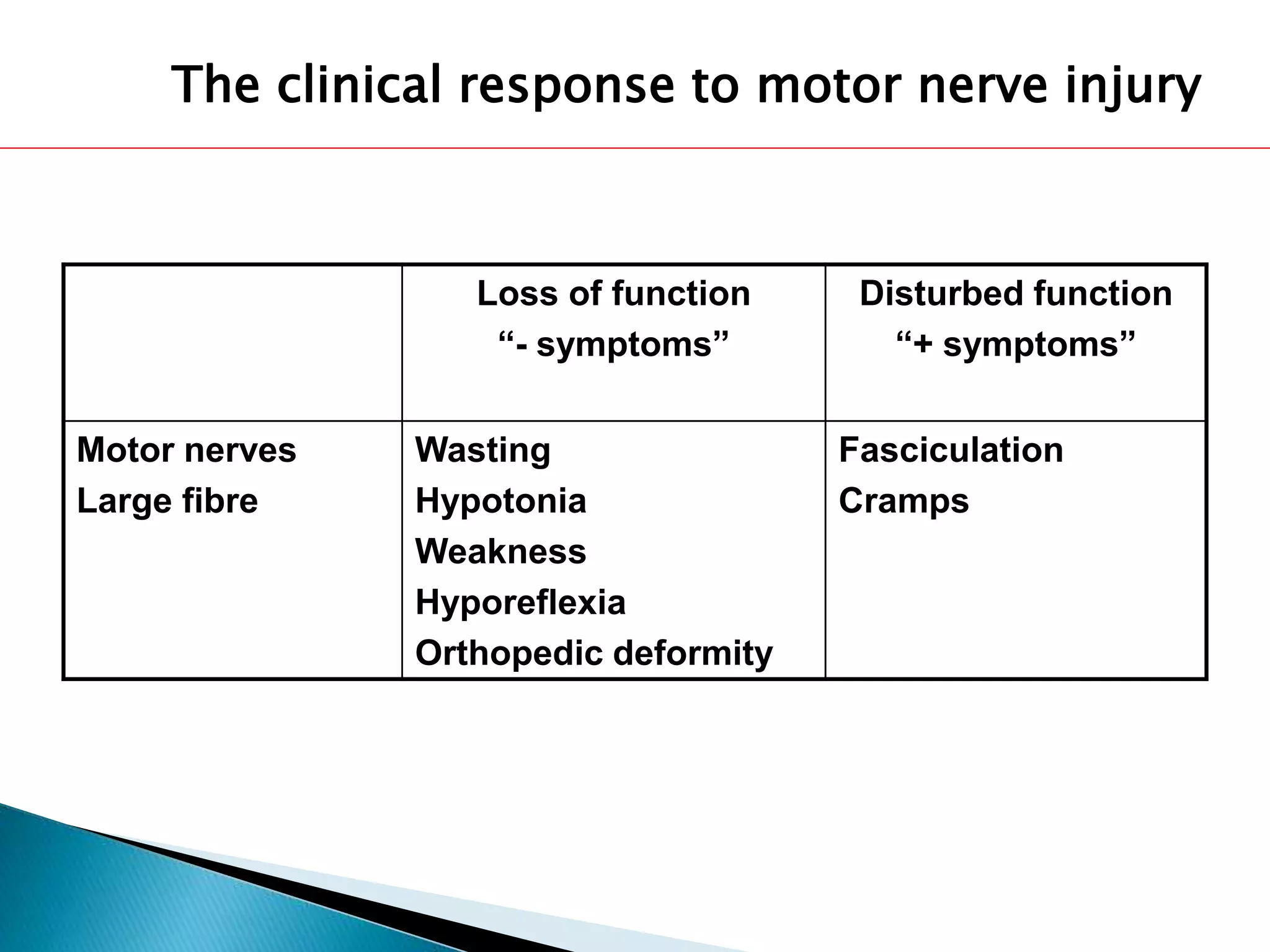
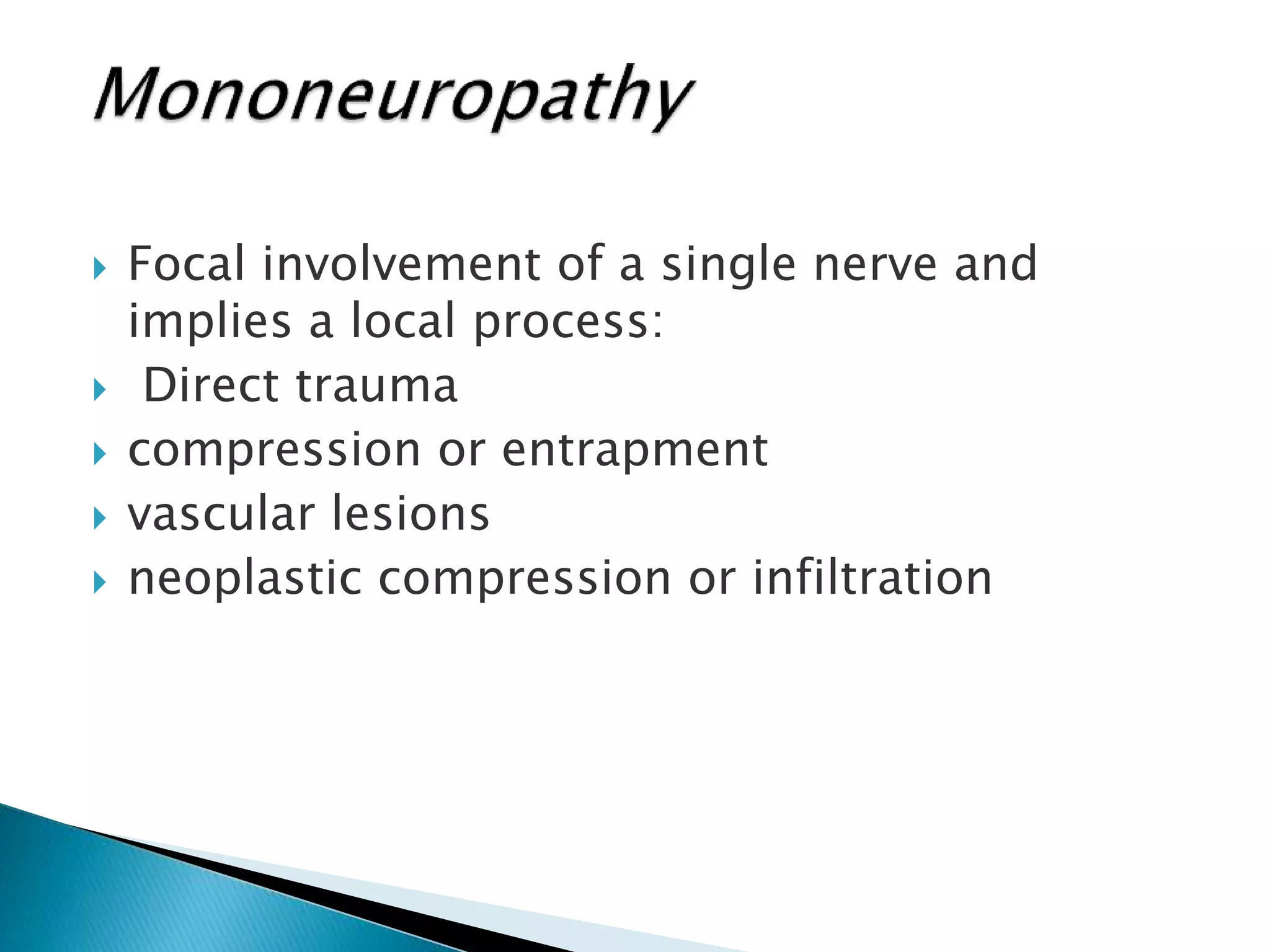
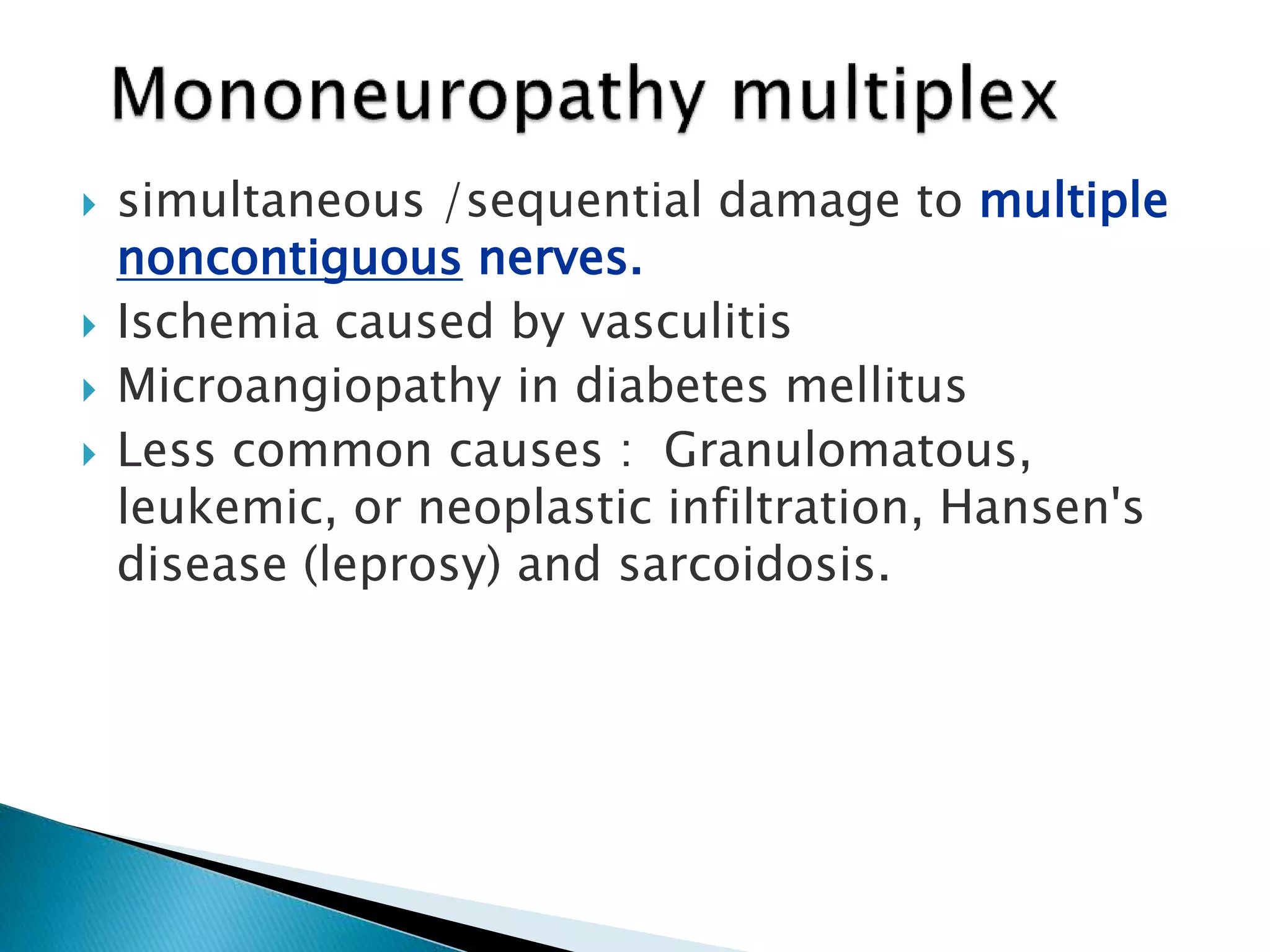
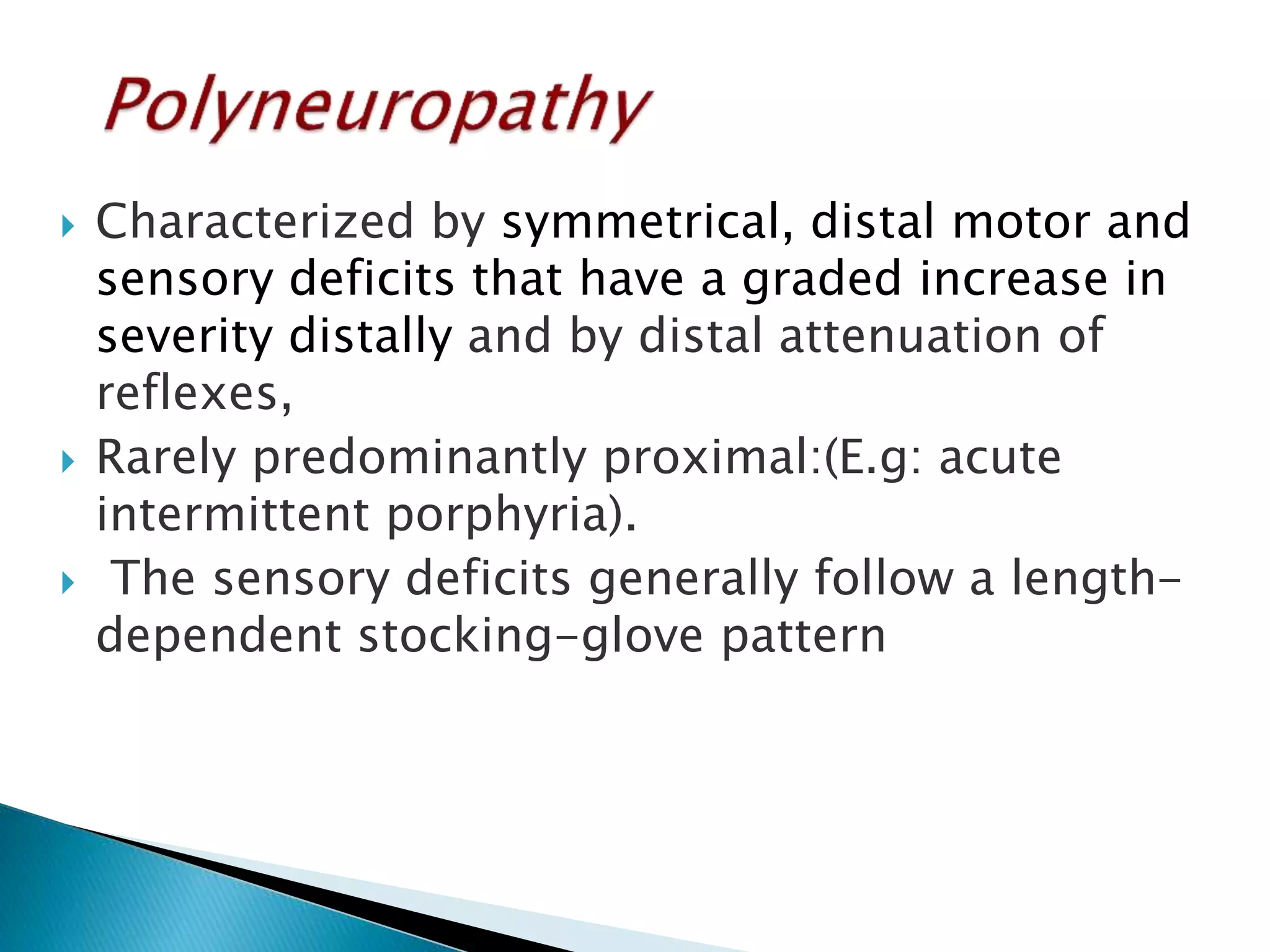
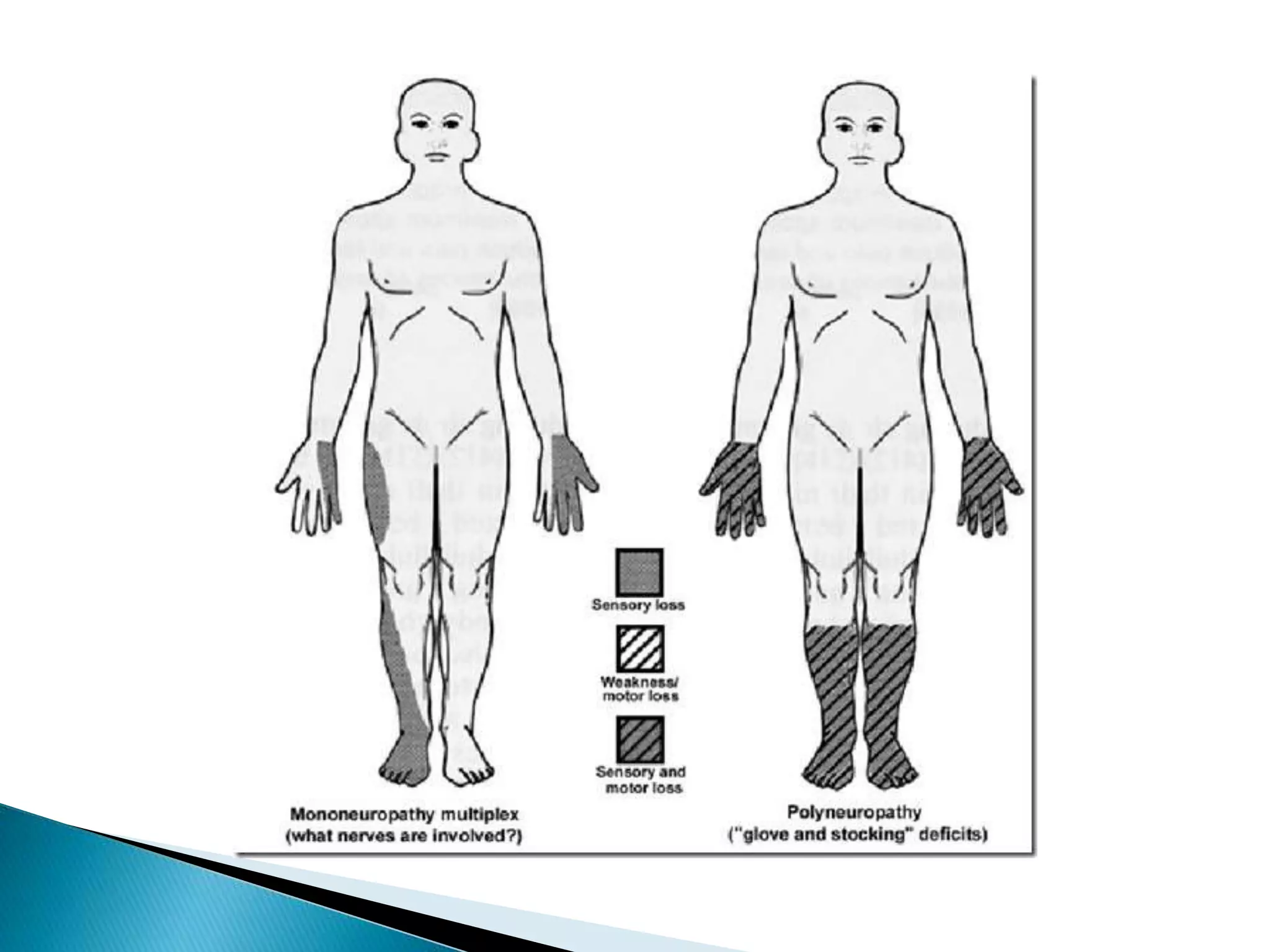
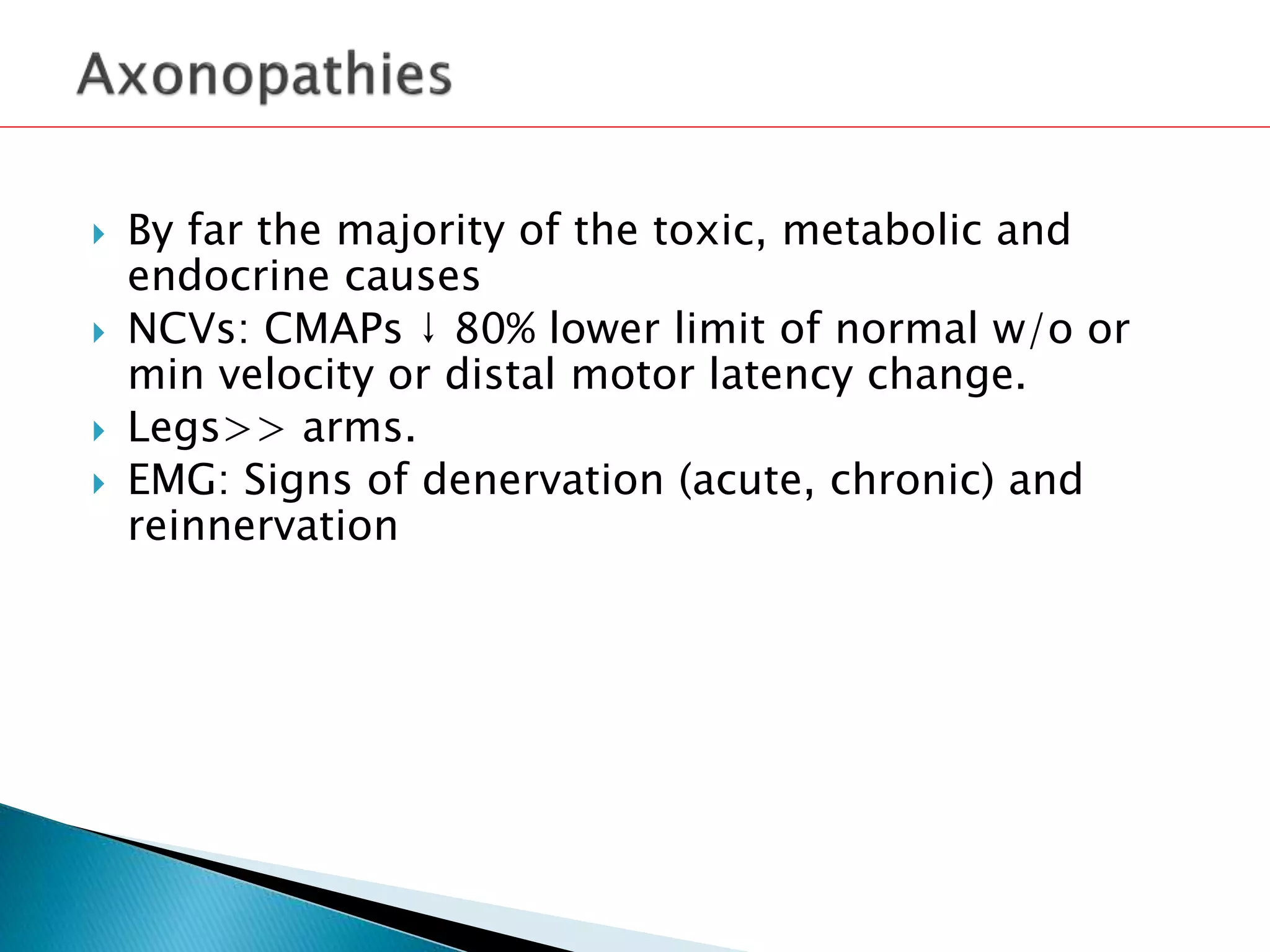
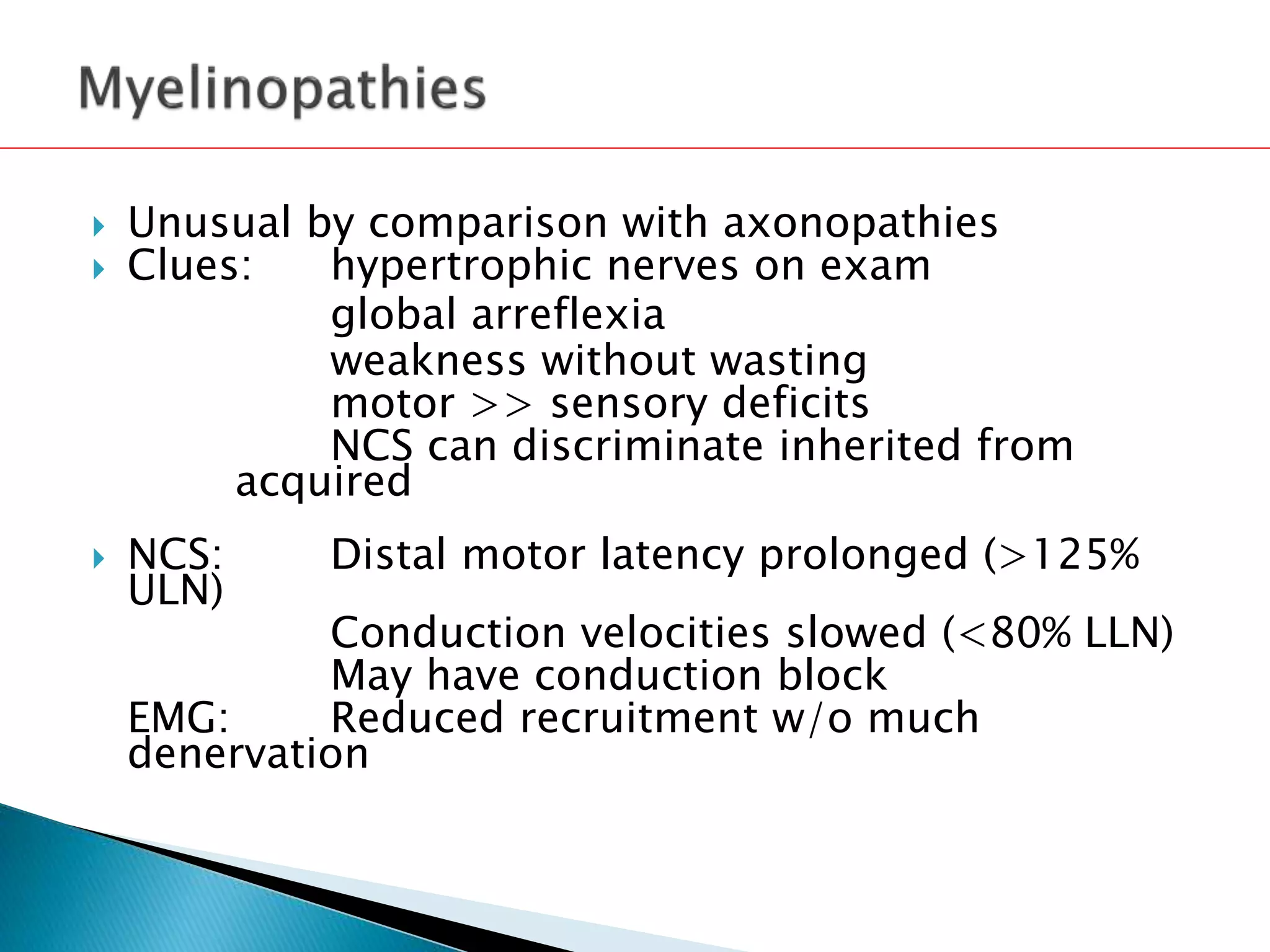
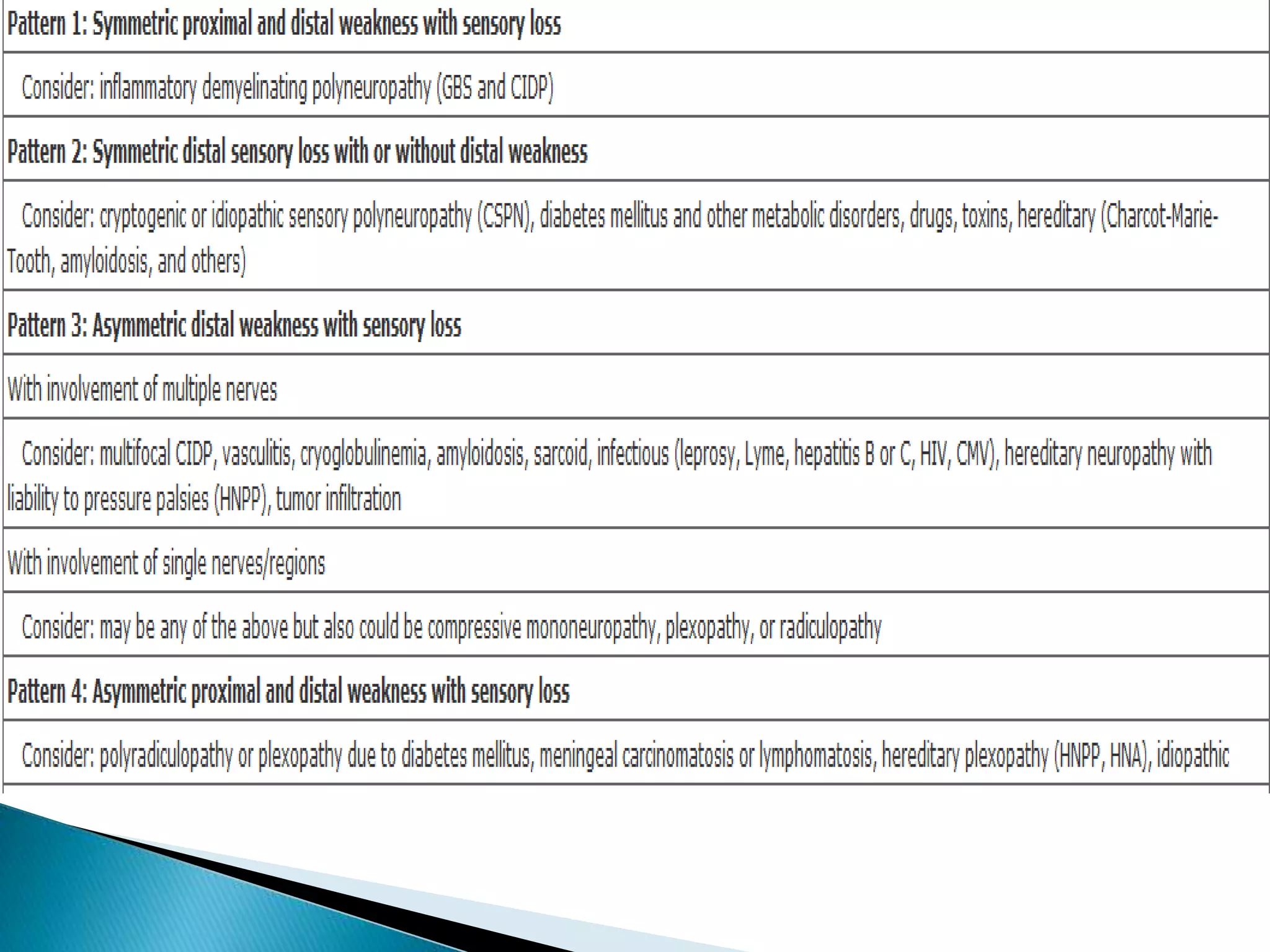
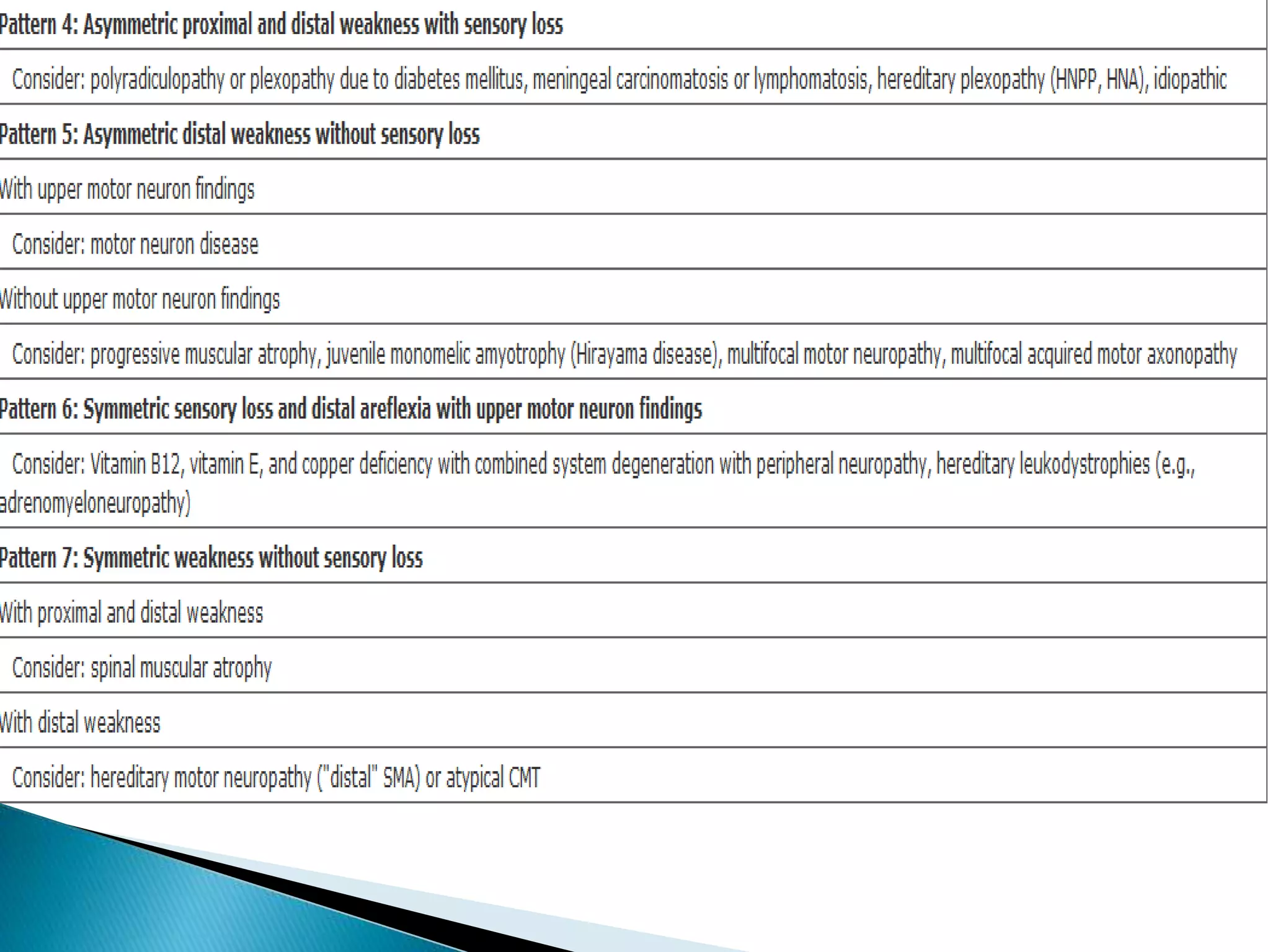
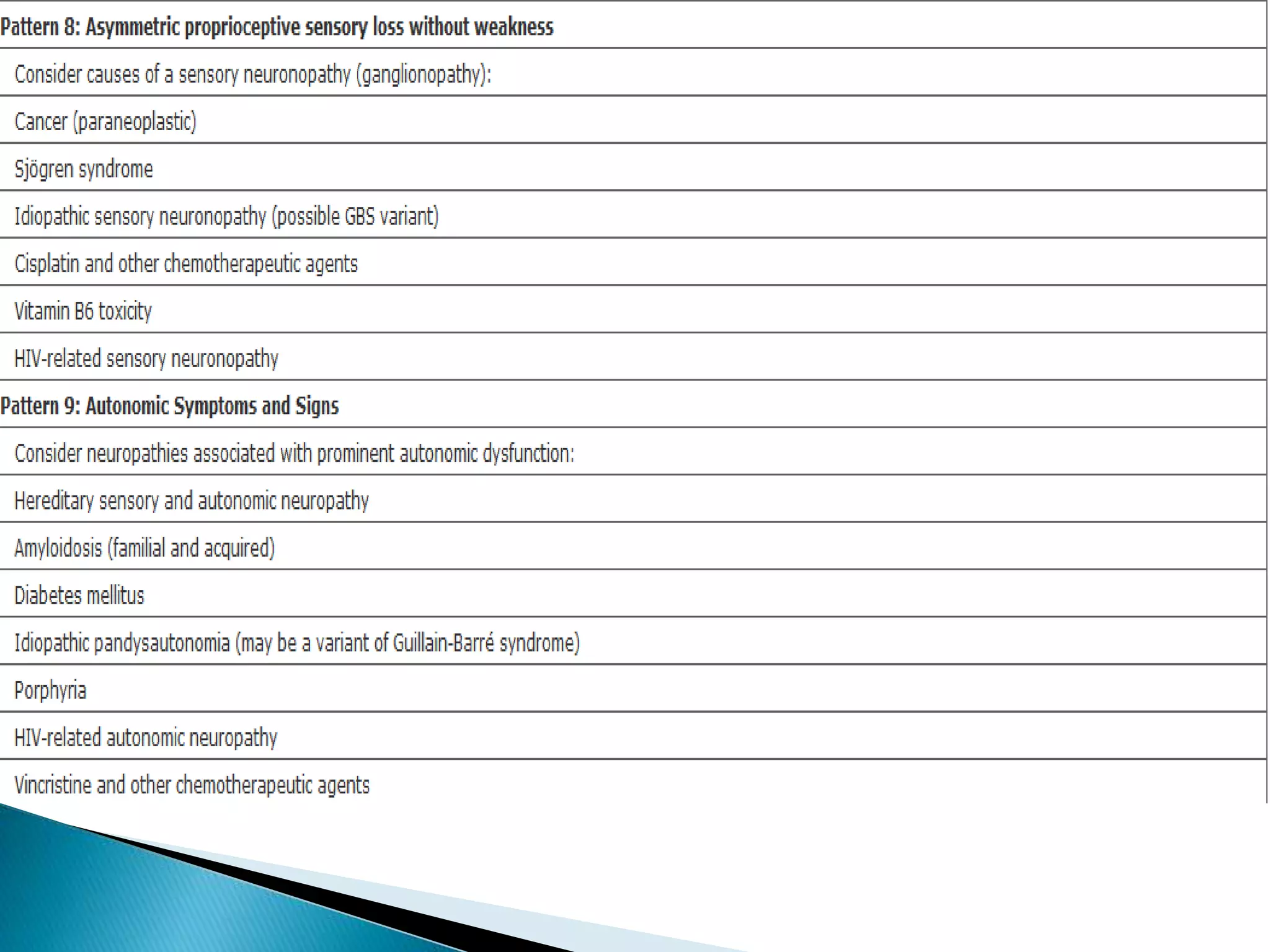
This document discusses peripheral neuropathy and provides guidance on evaluating and diagnosing peripheral nerve disorders. It defines peripheral neuropathy as disorders affecting the peripheral nervous system, which can involve sensory nerves, motor nerves, or both. The document outlines that peripheral neuropathies can be classified based on whether they primarily affect the cell body, myelin, or axon. It also lists common causes of peripheral neuropathy like diabetes, paraproteinemia, alcohol misuse, and vitamin B12 deficiency. The document provides guidance on clinical assessment, laboratory and electrodiagnostic testing, skin or nerve biopsy, and treatment approaches for peripheral neuropathy.
![ DM
•Weight loss, malaise, and anorexia.
hypothyroidism
chronic renal failure
liver disease
intestinal
malabsorption
malignancy
connective tissue
diseases
[HIV]
drug use
Vitamin B6 toxicity
alcohol and dietary
habits](https://image.slidesharecdn.com/approachtoperipheralneuropathy-140921053534-phpapp02/75/Approach-to-peripheral-neuropathy-18-2048.jpg)