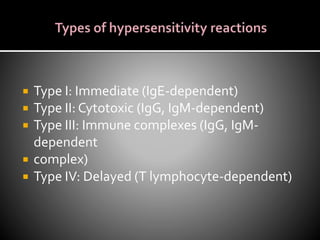
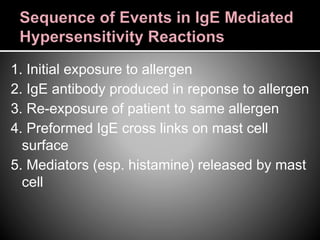
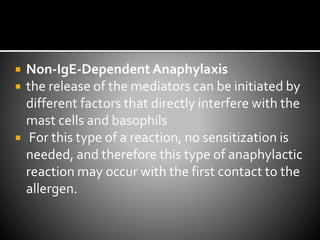
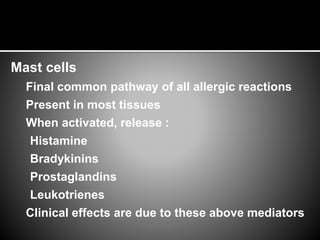
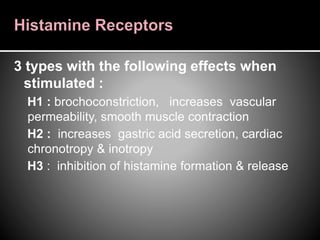
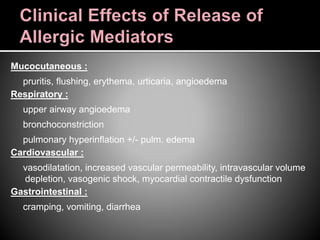
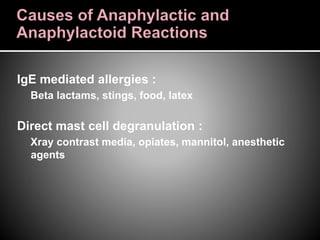
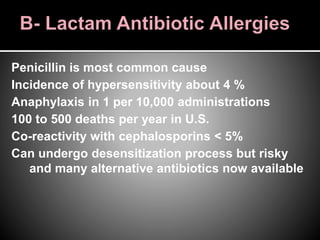
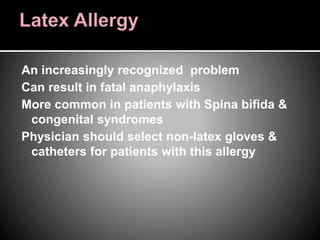
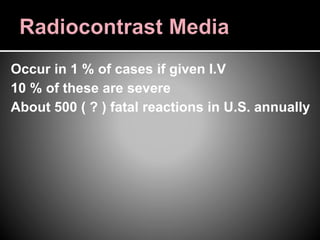
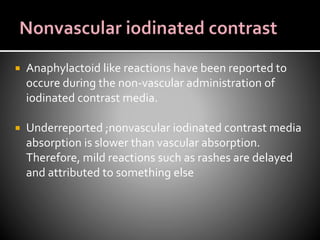
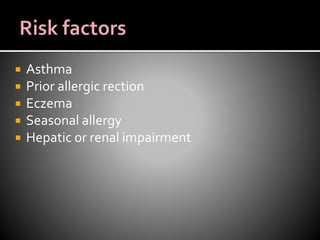
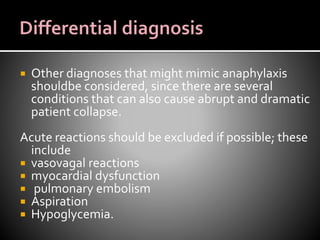
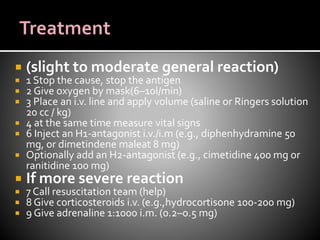
Anaphylaxis is a severe, life-threatening allergic reaction caused by the sudden release of mast cell and basophil mediators. It can be triggered by IgE-mediated or non-IgE mediated mechanisms. Common triggers include medications like antibiotics and contrast dyes, as well as stings, foods and latex. Symptoms affect multiple organ systems like the skin, respiratory and cardiovascular systems. Treatment involves stopping the trigger, supportive care, and medications like epinephrine, antihistamines and corticosteroids. Patients require monitoring for 24 hours due to risk of recurrence or delayed reactions.