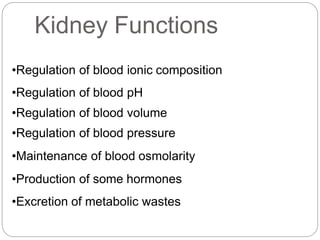
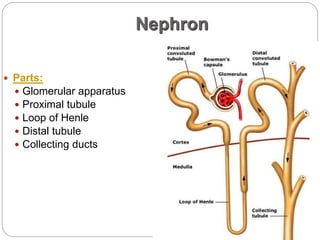
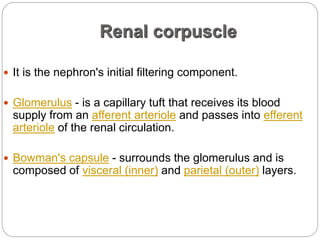
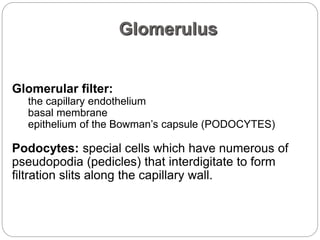
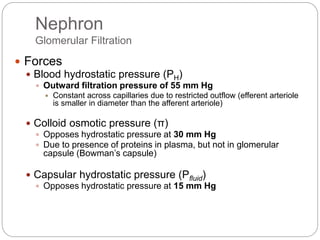
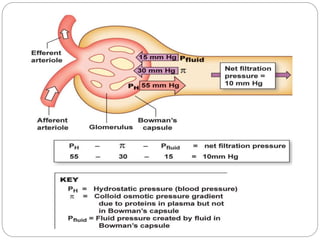
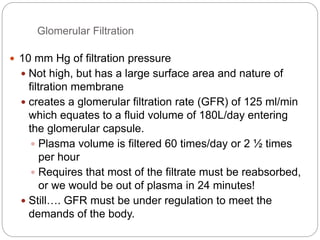
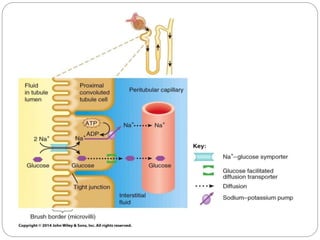
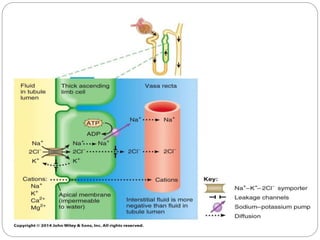
The kidney has several important functions including regulating blood pressure, fluid balance, and blood pH. The basic structural and functional unit of the kidney is the nephron, which filters blood to form urine. Each nephron contains a glomerulus for blood filtration and tubules (proximal tubule, loop of Henle, distal tubule, collecting duct) for reabsorption and secretion. Filtration occurs due to blood pressure gradients, with most filtrate reabsorbed along the nephron. The kidneys also produce hormones like renin, prostaglandins, and erythropoietin to help regulate blood pressure, red blood cell production, and other processes.