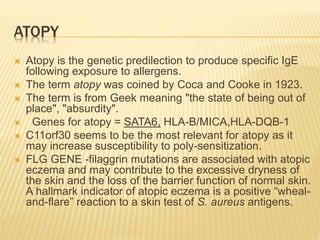
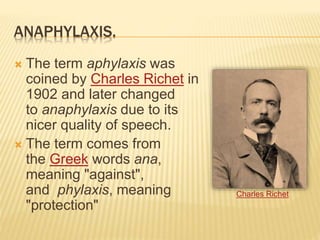
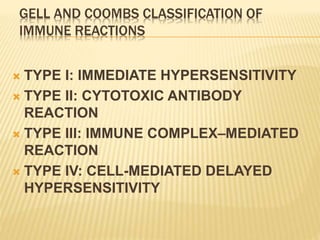
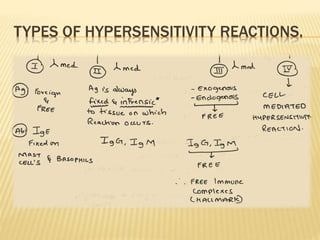
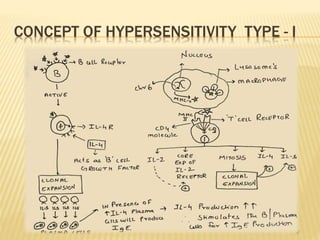
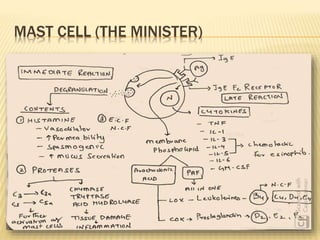
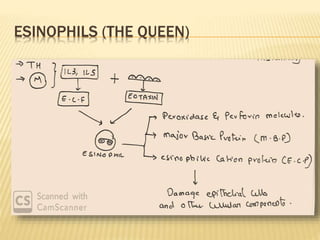
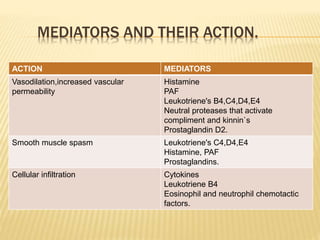
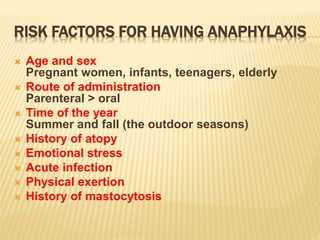
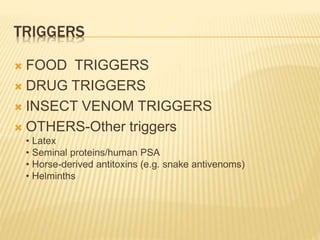
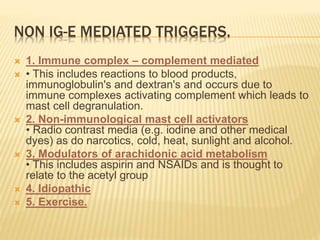
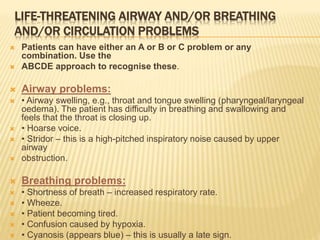
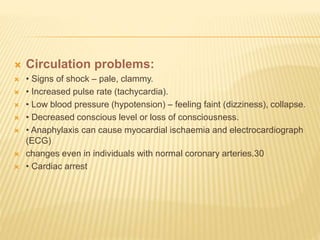
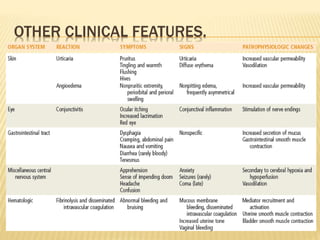
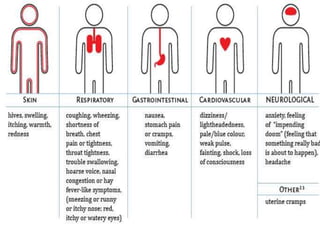
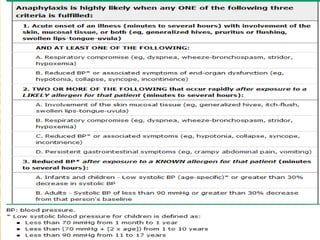
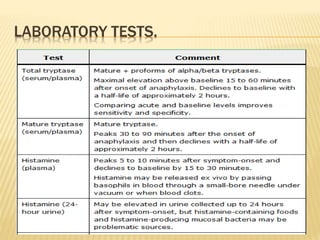
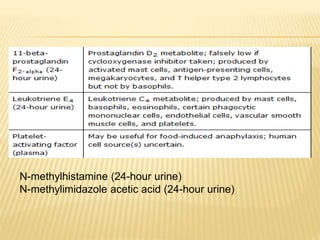
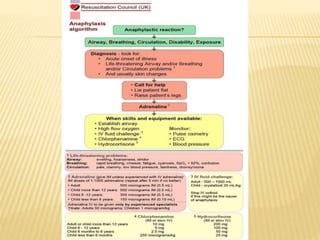
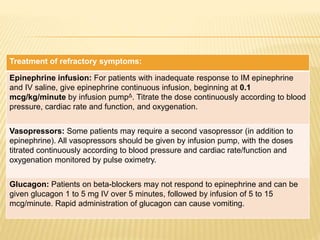
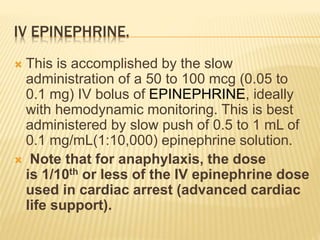
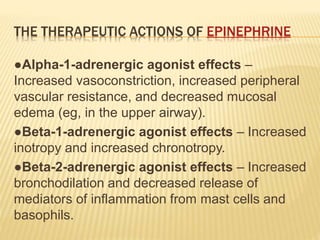
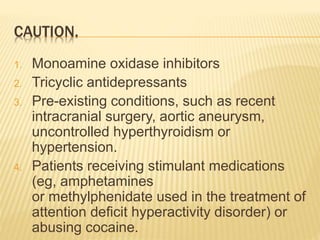
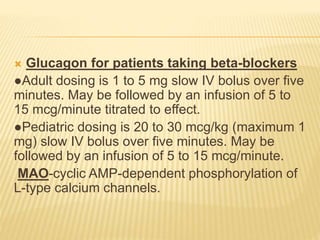
The document discusses atopy, allergies, and anaphylaxis, detailing the genetic predisposition to produce IgE in response to allergens and the classification of hypersensitivity reactions. It highlights the clinical significance of immediate reactions and the various factors and triggers leading to anaphylaxis, along with its life-threatening symptoms. Additionally, the document outlines treatment options for anaphylaxis, including epinephrine and glucagon, while noting precautions and considerations for specific patient populations.