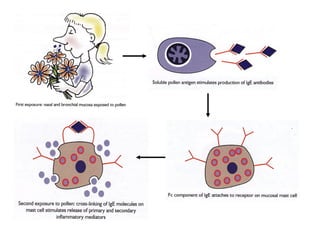
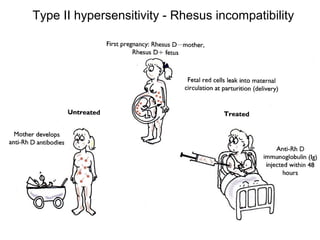
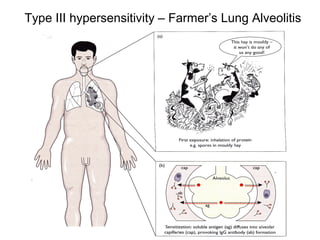
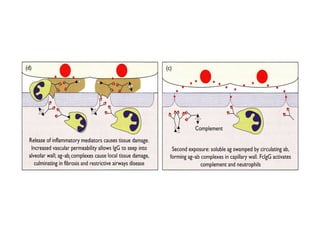
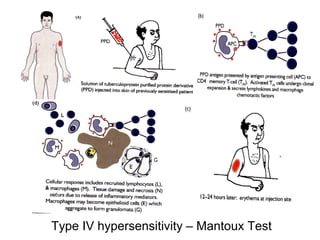
This document discusses hypersensitivity reactions and autoimmune diseases. It describes the different types of hypersensitivity reactions (Type I-IV) and their mechanisms and examples. It also discusses autoimmune diseases, noting they arise due to genetic susceptibility and environmental triggers damaging self tolerance. Autoimmune diseases can affect many organ systems. The document also briefly touches on tissue transplant rejection, immunodeficiencies, HIV/AIDS, and amyloidosis.