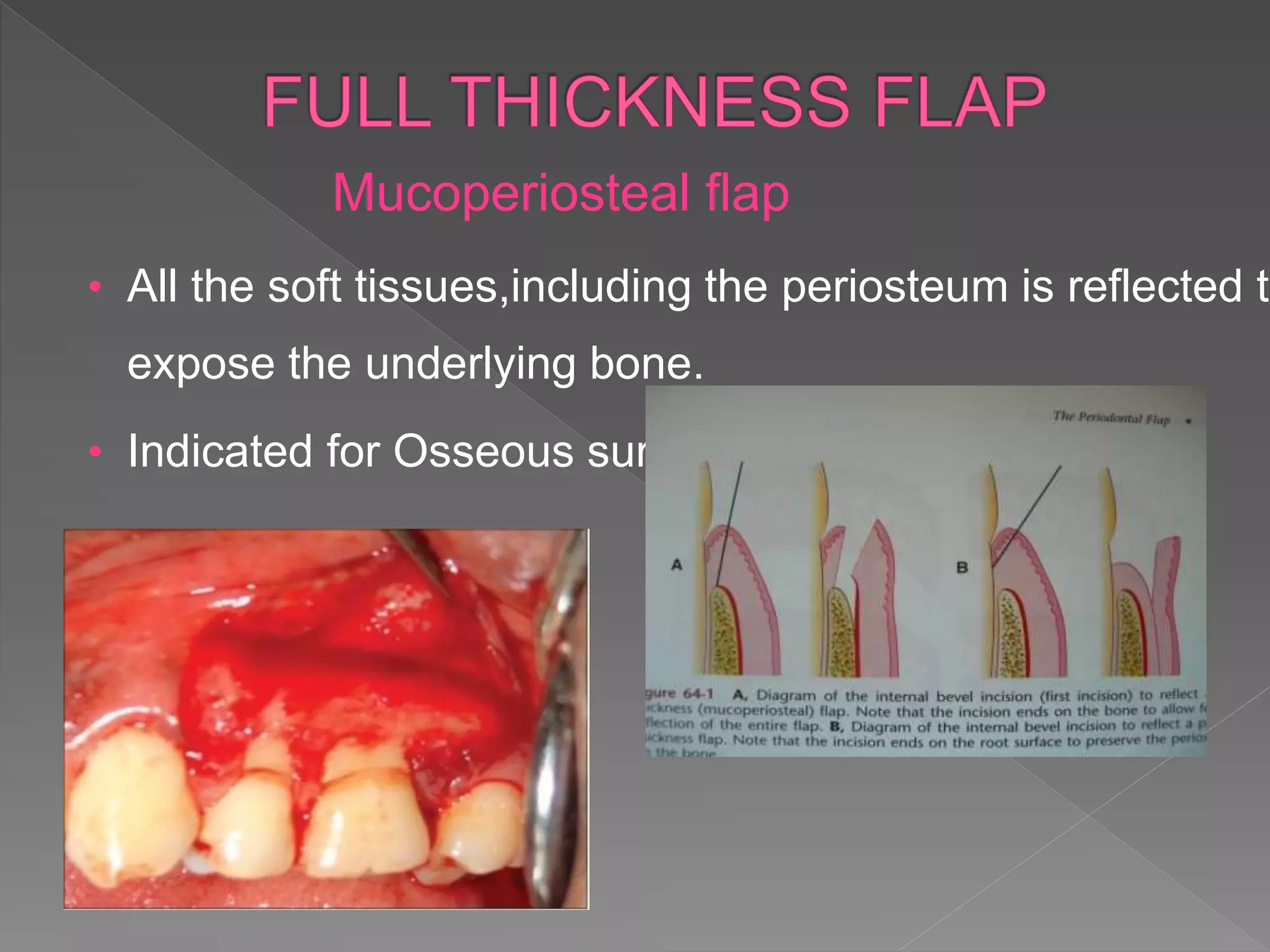
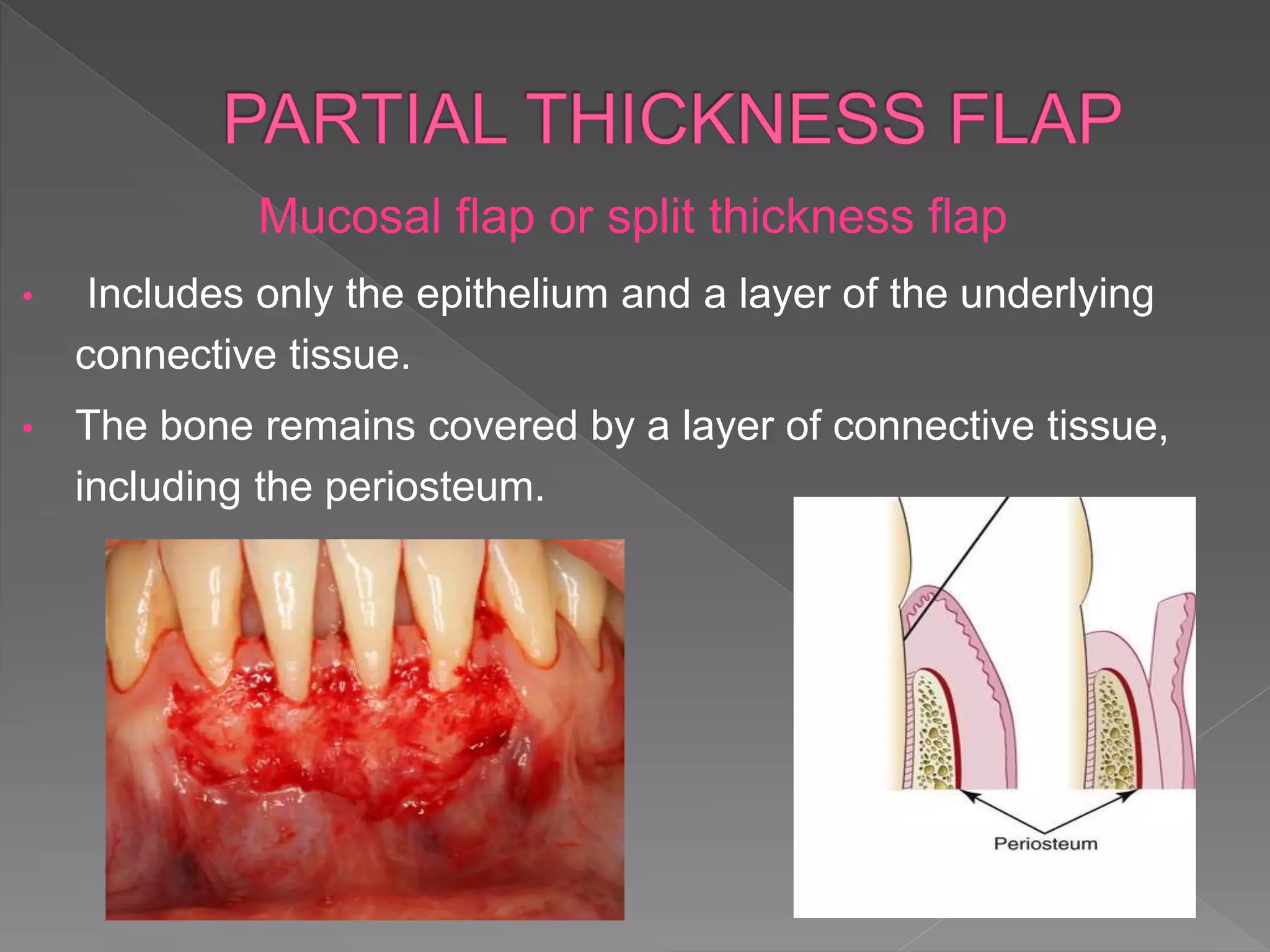
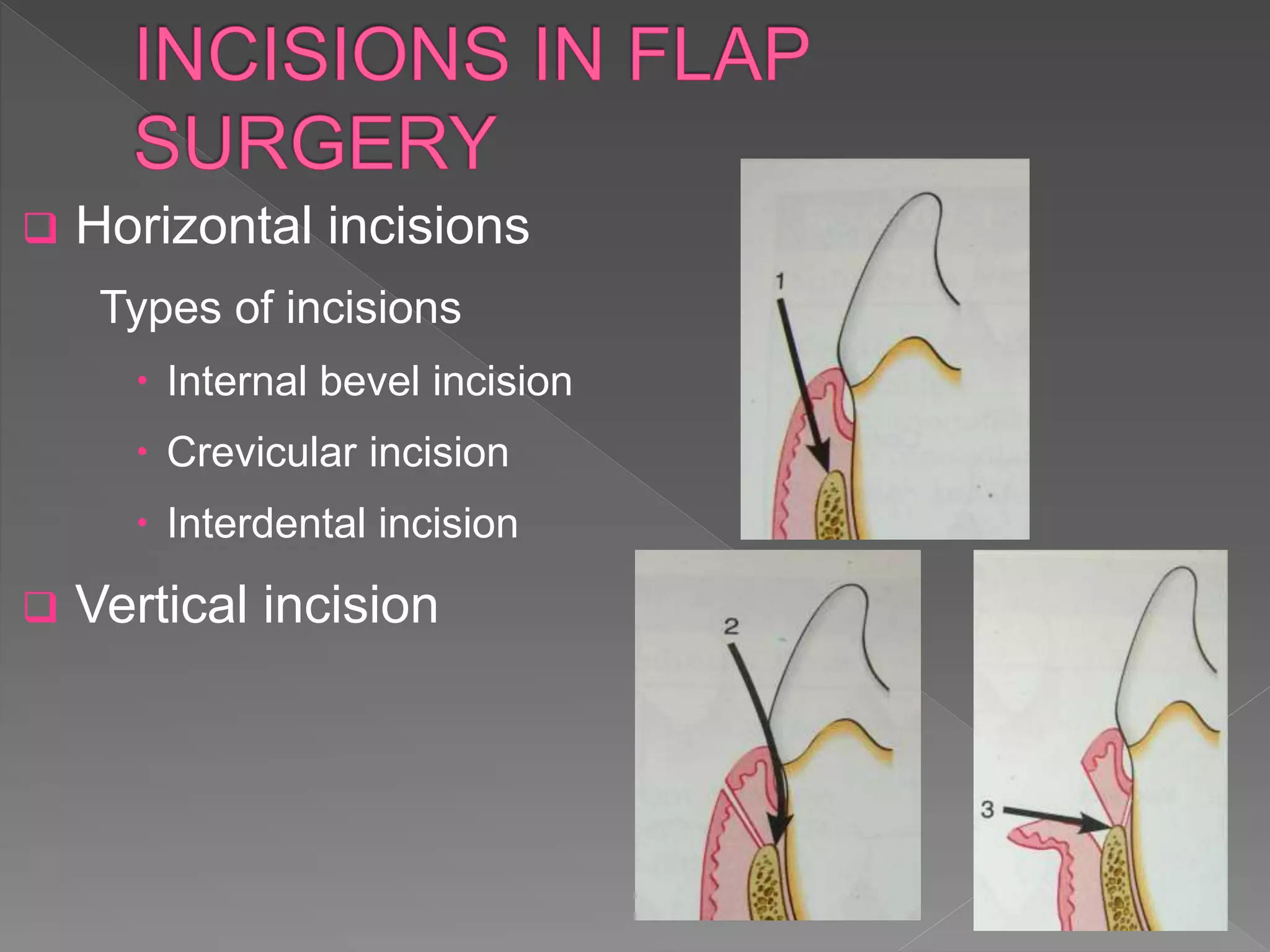
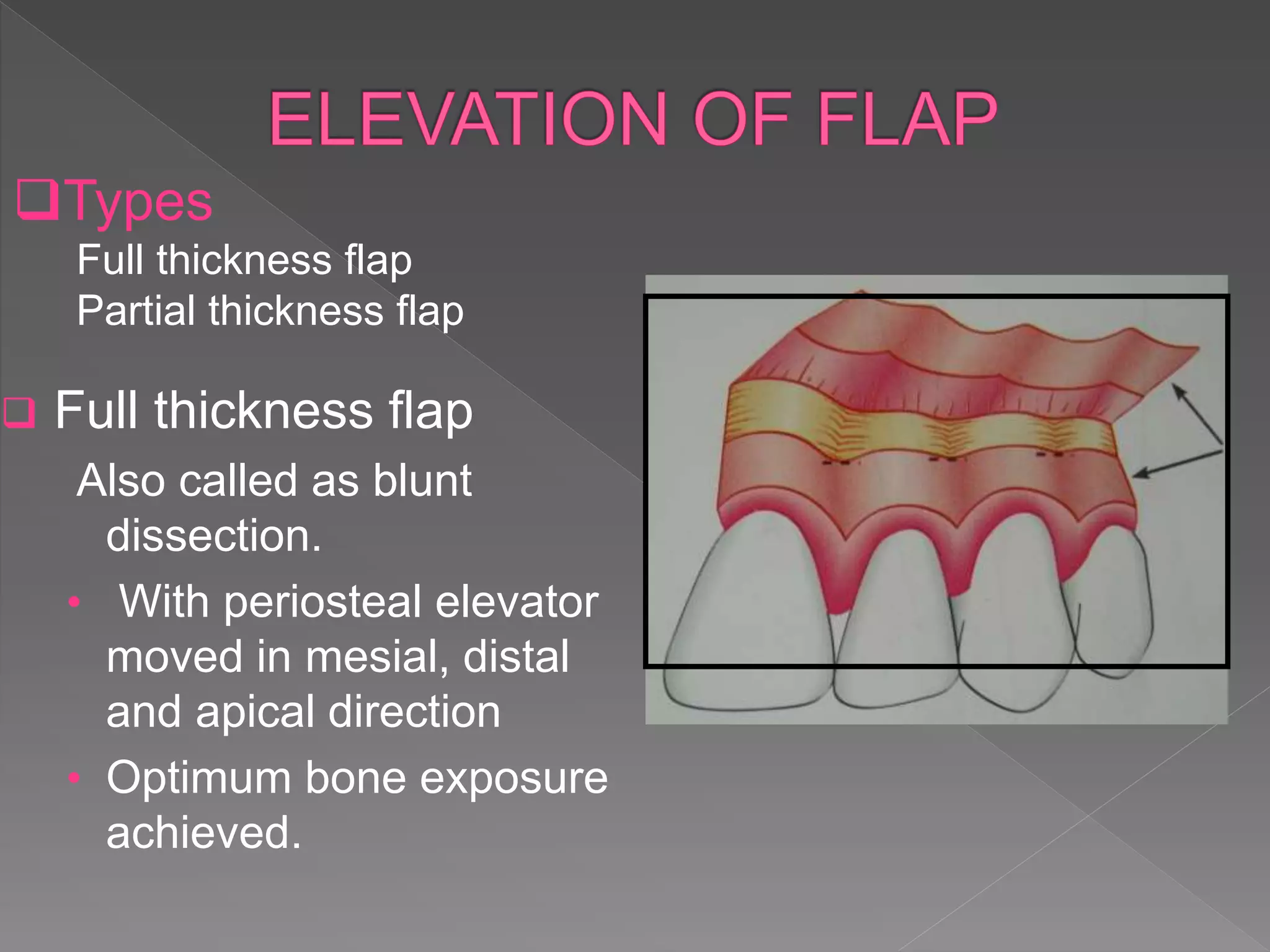
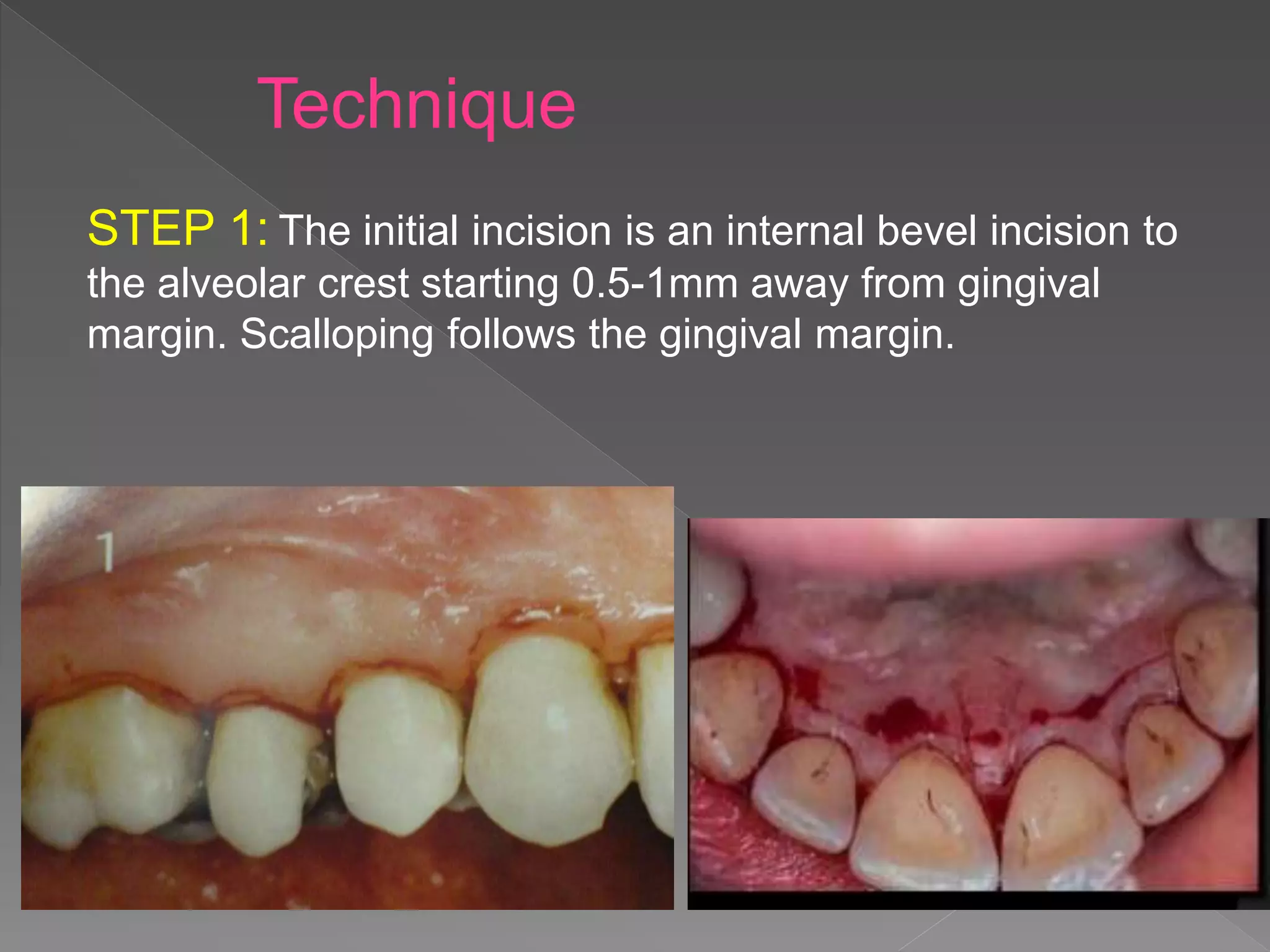
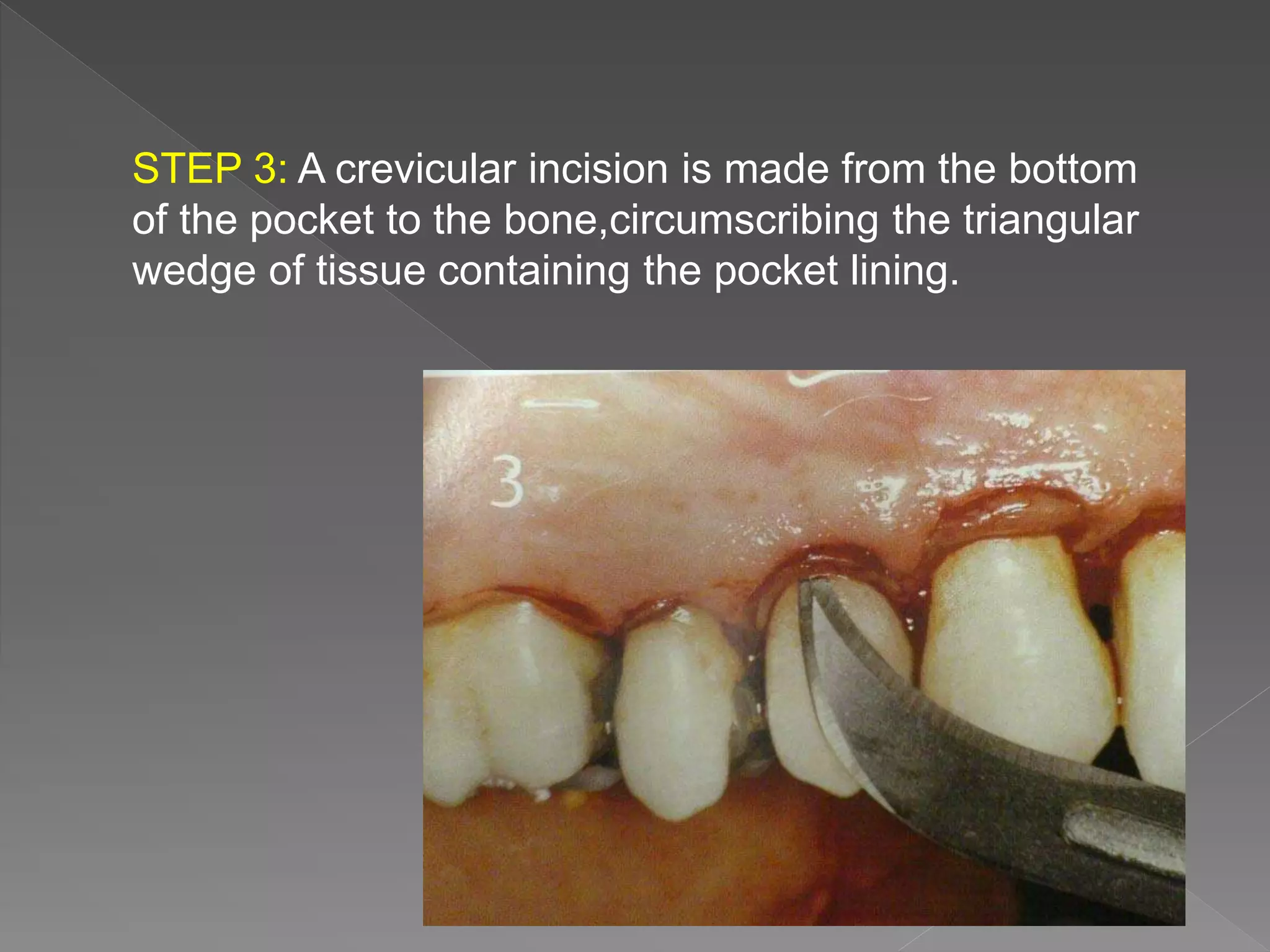
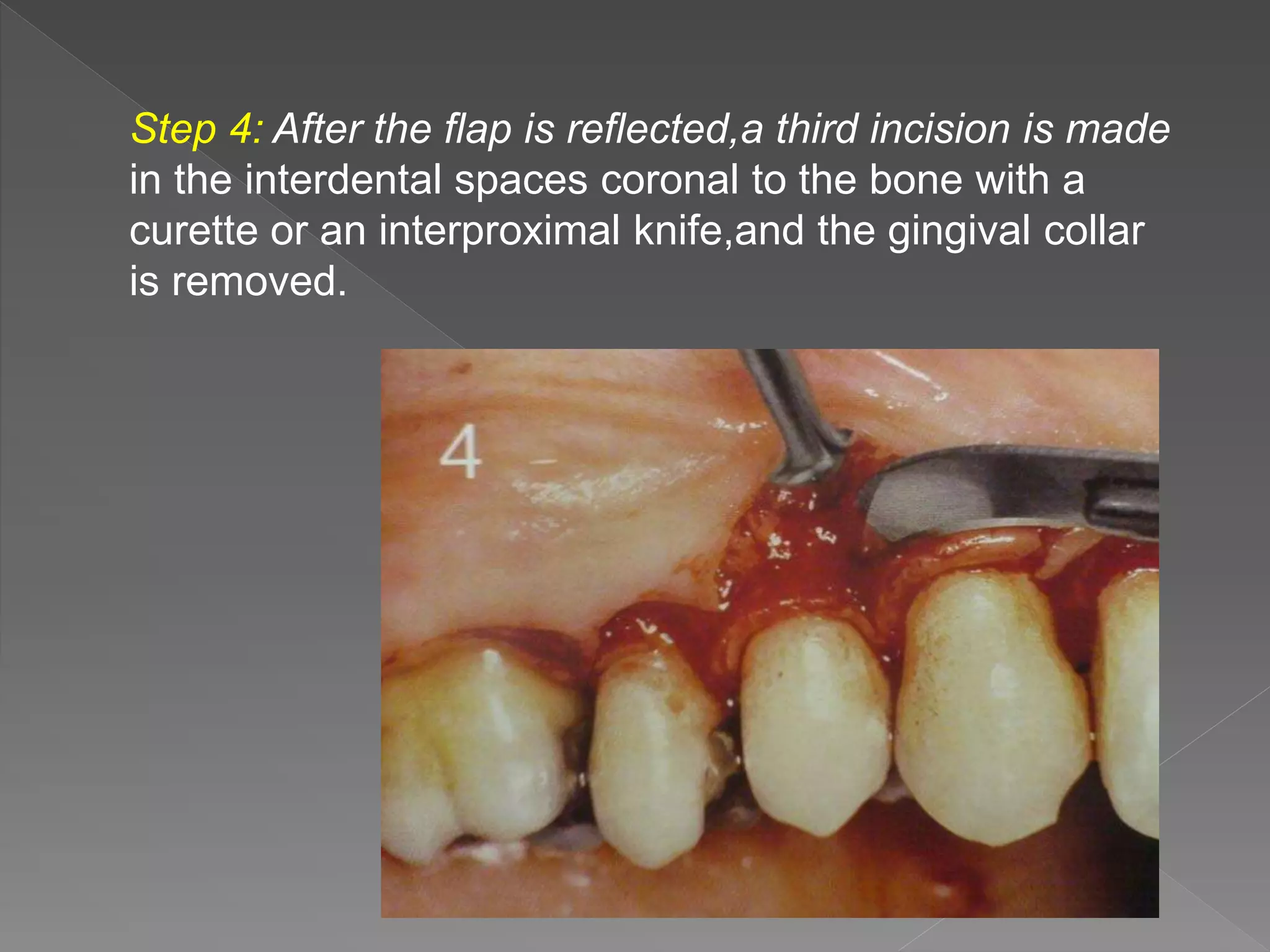
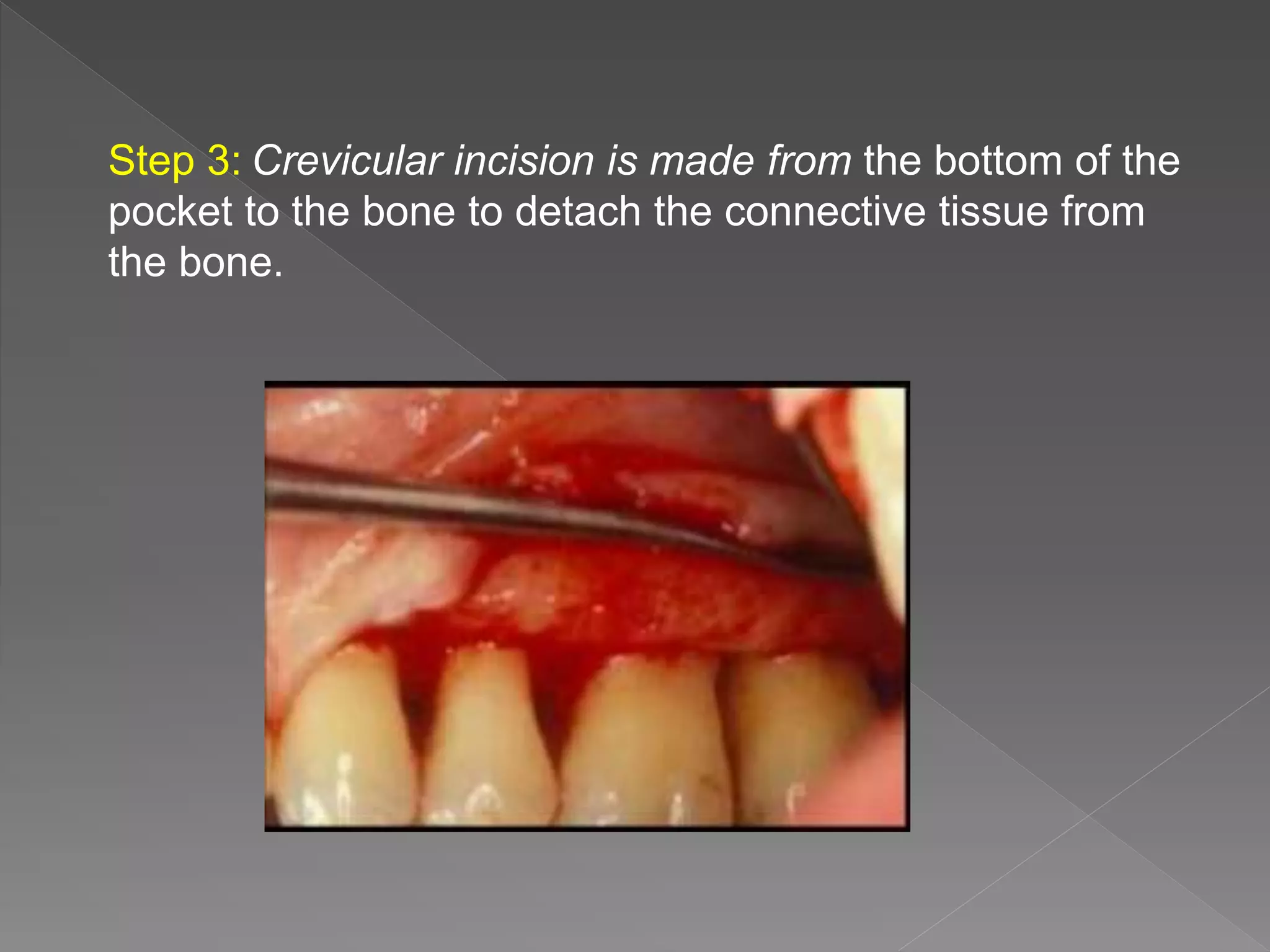
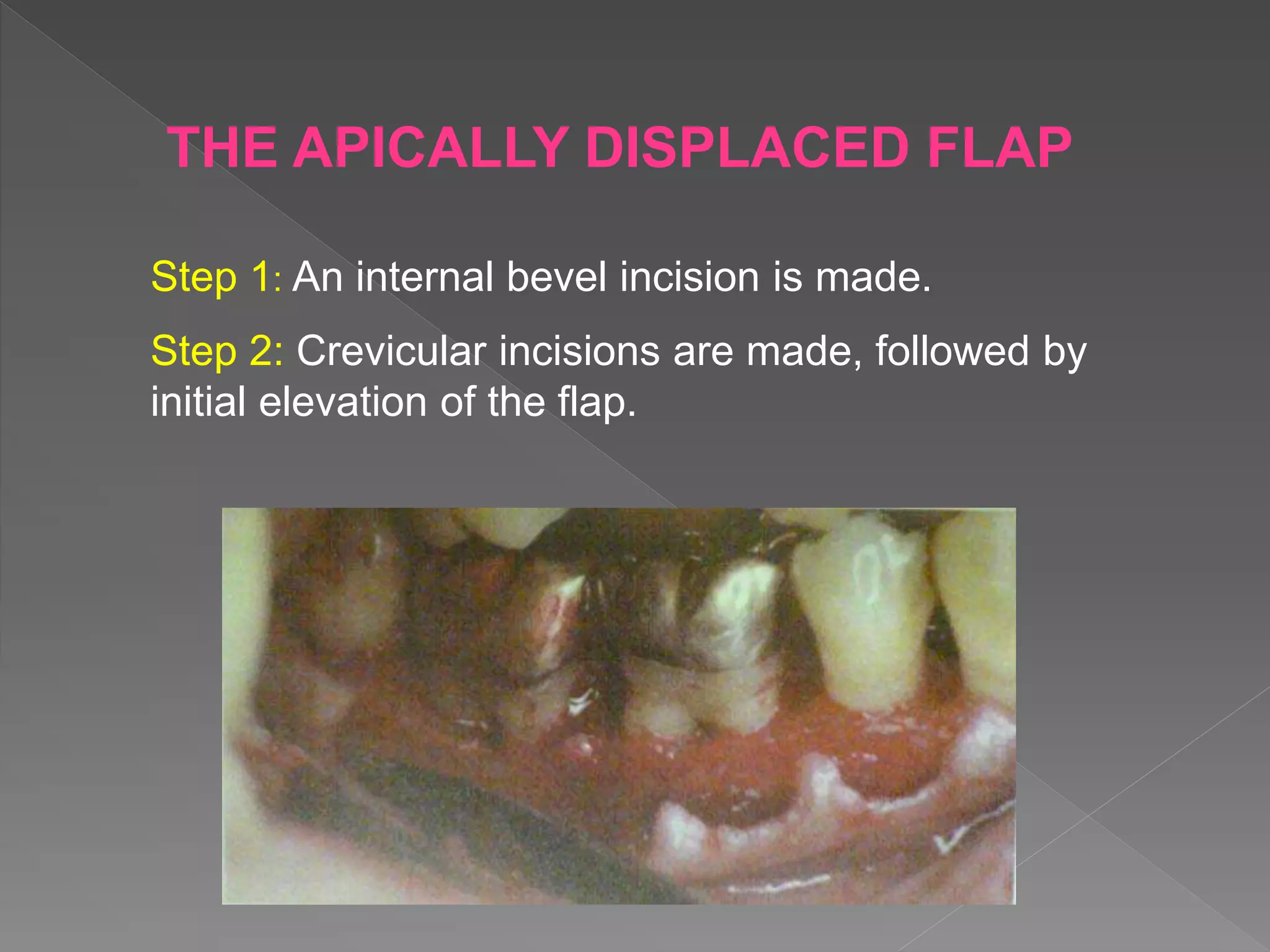
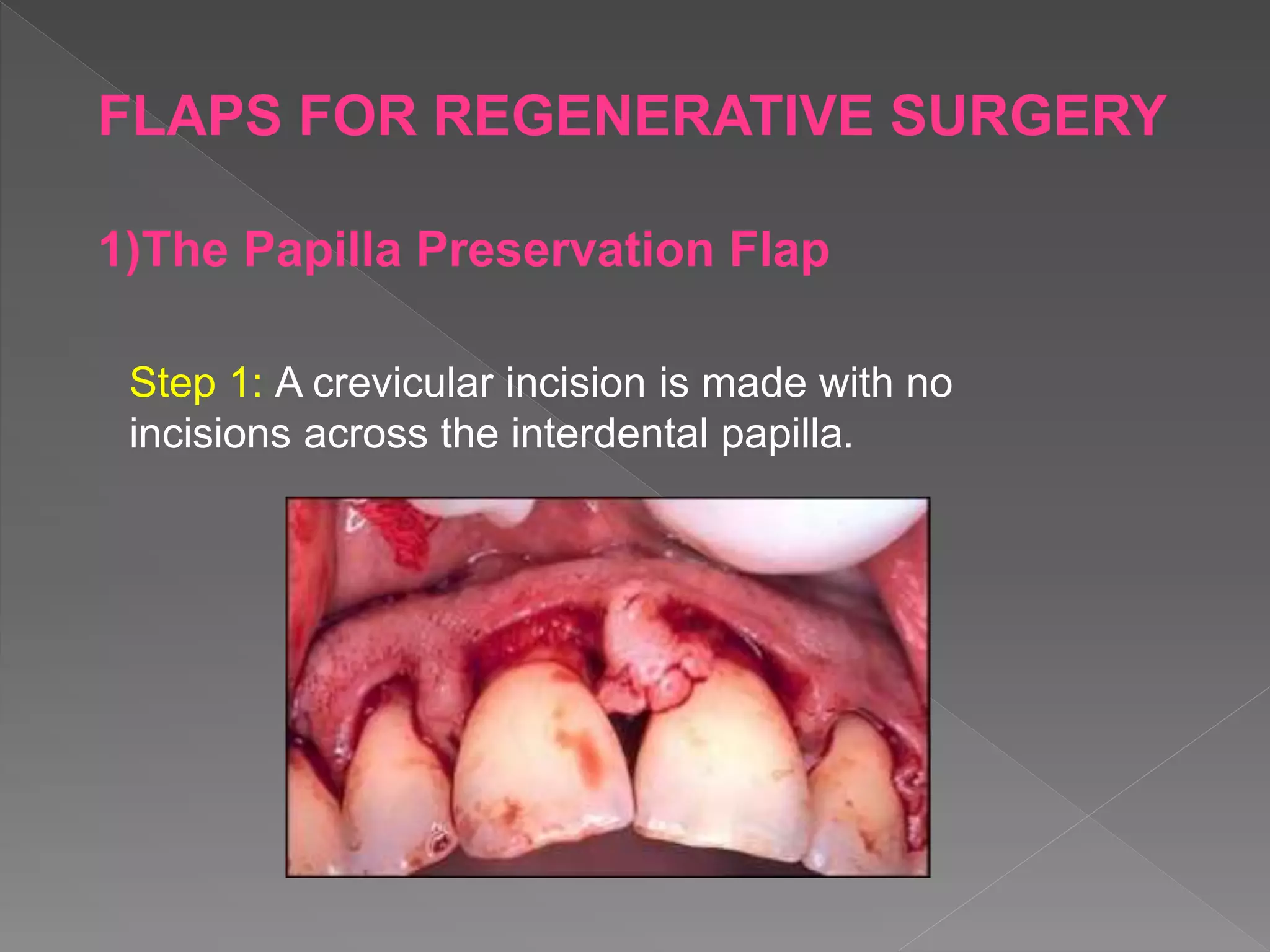
This document discusses various flap techniques used in periodontal surgery. It defines flaps as sections of gingiva and mucosa surgically separated from underlying tissues to provide access to bone and roots. Full and partial thickness flaps are classified based on the depth of tissue reflection. Techniques include the modified Widman flap, undisplaced flap, apically displaced flap, papilla preservation flap, and techniques for distal molar surgery. Healing after flap surgery is described in stages from initial clot formation to establishment of new connective tissue attachment after 4 weeks.