Periodontal Pocket
- 1. Presented by: Dr. Kishlay Bhartiya JR-III Department of Periodontology F.O.D.S., K.G.M.U., Lucknow
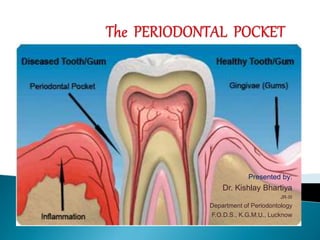
- 2. The periodontal pocket is defined as a pathologically deepened gingival sulcus, and it is one of the most important clinical features of the periodontal disease.
- 3. 1. Coronal movement of gingival margin 2. Apical displacement of the gingival attachment 3. A combination the two process As Deepening of gingival sulcus may occur by: -
- 4. Pockets can be classified as follows : 1. Gingival Pocket (Pseudopocket) – formed by gingival enlargement without destruction of the underlying tissues. The sulcus is deepened because of the increased bulk of the gingiva. 2. Periodontal Pockets – it occurs with destruction of supporting periodontal tissues. Two types of periodontal pockets exist : I. Suprabony (Supracrestal or Supraalveolar) - In this, bottom of the pocket is coronal to the underlying alveolar bone. II. Intrabony (Infrabony, Subcrestal or intraalveolar) - In this, bottom of the pocket is apical to the level of the adjacent alveolar bone and the lateral pocket wall lies between the tooth surface & alveolar bone.
- 5. A. Gingival Pocket B. Suprabony C. Intrabony Pocket
- 6. Periodontal pockets can also be classified- [A] According to involved tooth surface 1. Simple 2. Compound 3. Complex or Spiral – originating on one surface and twisting around the tooth to involve one or more additional surfaces ( most commonly found in furcation area) I II III
- 7. [B] Depending upon the nature of the soft tissue wall of the pocket: (1) Edematous Pocket. (2) Fibrotic Pocket. [C] Depending upon disease activity: (1) Active Pocket. (2) Inactive Pocket.
- 8. SIGNS : 1) Bluish red, thickened marginal gingiva. 2) A Bluish red vertical zone from the gingival margin to alveolar mucosa. 3) Gingival bleeding and suppuration. 4) Tooth mobility. 5) Diastema formation. 6) A rolled edge separating the gingiva Margin from the tooth surface. 7) A break in the facio-lingual continuity of interdental gingiva. 8) Shiny, puffy gingiva leads to exposed root surface.
- 9. SYMPTOMS 1) Localized pain or “pain deep in the bone” 2) Usually painless but may give rise to localized / radiating pain or sensation of pressure after eating which gradually reduces. 3) A foul taste in localized areas. 4) Sensitivity to hot & cold. 5) Toothache in the absence of caries is also sometimes present. 6) A tendency to suck material inter proximally. 7) Feeling of itching in the gums. 8) Urge to dig a pointed instrument in the gums. 9) Feeling of loose teeth.
- 10. CLINICAL FEATURES 1. Bluish red discoloration of gingival pocket wall 2. Flaccidity 3. Smooth and shiny surface 4. Pitting on pressure 5. Less frequently gingival wall may be pink and firm 6. Bleeding on gentle probing 7. Inner wall of pocket is painful 8. Pus discharge on applying digital pressure HISTOPATHOLOGIC FEATURES 1. Circulatory strangulation 2. Destruction of gingival fibers and surrounding tissue 3. Atrophy of epithelium 4. Edema and degeneration 5. Fibrotic changes predominate over exudation and degeneration 6. Increased vascularity, thinning of epithelium and proximity of engorged vessels to inner surface. 7. Ulceration of inner aspect of pocket wall. 8. Suppurative inflammation of inner wall.
- 11. The only reliable method of locating periodontal pockets and determining their extent is careful probing along each tooth surface. There are two different pocket depths - Biologic or Histologic depth :- is the distance between the gingival margin and the base of the pocket (the coronal end of the junctional epithelium. Clinical or probing depth :- Is the distance from the gingival margin to which a probe penetrates in to the pocket. ◉ According to several investigators - The probing force of 0.75 N or 25 gm have been found to be well tolerated and accurate.
- 12. In normal sulcus, the probe penetrates about one third to one half the length of junctional epithelium In periodontal pocket with a short junctional epithelium the probe penetrates beyond the apical end of junctional epithelium.
- 13. Vertical insertion of the probe (Left) may not detect interdental craters, oblique positioning of the probe (Right) reaches the depth of the crater. Vertical Oblique
- 14. “Walking” the probe to explore the entire pocket
- 15. The initial lesion in the development of Periodontitis in response to a bacterial challenge is inflammation of the gingiva. o Changes involved in the transaction from the normal gingival sulcus to pathologic periodontal pocket are as follows: Inflammatory change occur in connective tissue wall of the gingival sulcus ↓ Cellular & inflammatory exudates cause degeneration of surrounding connective tissue & gingival fibers ↓ Collagen fibers are destroyed just apical to junctional epithelium ↓ Area becomes occupied by inflammatory cells & edema
- 16. There are two mechanisms of collagen loss I II Collagenases & other enzymes secreted by various cells such as fibroblasts, PMNs, leukocyte & macrophages, becomes extracellular and destroy collagen; these enzymes that degrade collagen and other matrix macro molecules into small peptides are called matrix metalloproteinases. Fibroblasts phagocytize collagen fibers by extending cytoplasmic process to the ligament-cementum interface and degrade the inserted collagen fibrils and the fibrils of the cementum matrix.
- 17. After collagen loss, apical cells of Junctional Epithelium proliferate along the root, extending finger like projections two or three cells in thickness. ↓ Coronal portion of Junctional Epithelium detaches from the roots as the apical portion migrates. ↓ As a result of inflammation PMNs invades the coronal end of Junctional Epithelium and when relative volume becomes approx. 60% or more of the Junctional Epithelium, the tissue looses cohesiveness & detaches from the tooth surface. Area of destroyed collagen at base of the pocket and thin fingerlike extension of epithelium covering the cementum
- 18. Some Important Points Extension of Junctional Epithelium along the root requires the presence of healthy viable, epithelial cells and so it is reasonable to assume that the degenerative changes seen in this area occur after the junctional epithelium reaches its position on cementum. The degree of leukocyte inflammation of junctional epithelium is independent of the volume of inflamed connective tissue. The transformation of a gingival sulcus into a periodontal pocket creates an area where plaque removal becomes impossible and following feedback mechanism is established:- Plaque Accumulation Gingival Inflammation Pocket Formation Area difficult to clean
- 19. Once the pocket is formed, several microscopic features are present and discussed in following sections:- Changes in the soft tissue wall: The connective tissue is edematous & densely infiltrated with plasma cells (approx. 80%), lymphocytes & a scattering of PMNs. Blood vessels are increased in number, dilated and engorged particularly in the subepithelial connective tissue layer. Connective tissue exhibit varying degrees of degeneration. The connective tissue shows proliferation of endothelial cells with newly formed capillaries, fibroblasts and collagen fibres. The Junction Epithelium at the base of the pocket is usually much shorter than that of a normal sulcus and usually coronoapical length of junctional epithelium is reduced to only 50-100 m.
- 20. Changes along the lateral wall : Most severe degenerative changes occur along lateral wall. The epithelium presents striking proliferative & degenerative changes . Epithelial buds or interlacing cords of epithelial cells project from lateral wall into adjacent inflamed connective tissue & may extend farther apically to Junctional Epithelium. These epithelium projection and remainder of lateral epithelium are densely infiltrated by Leukocytes and edema from the inflamed connective tissue. These cells can undergo vacuolar degeneration and rupture to form vesicles. Progressive degeneration & necrosis of epithelium lead to Ulceration of lateral wall,Exposure of inflamed connective tissue and suppuration. The severity of degenerative changes are not necessarily related to pocket depth. Ulceration may occur in shallow pockets and deep pockets with intact lateral epithelium is rarely observed. The Epithelium at the gingival crest of a periodontal pocket is generally intact & thickened, with prominent rete pegs.
- 21. Lateral wall showing epithelial proliferation and atrophic changes Base of the pocket showing extensive proliferation of lateral epithelium
- 22. Bacterial Invasion Occurs along the lateral & apical areas of the pocket in cases of chronic periodontitis. Filaments, Rods & coccoid organisms with predominent gram- negative cell walls have been found in intercellular spaces of epithelium. Hillmann et al reported presence of Porphyromonas gigivalis and Prevotella intermedia in the gingiva of aggressive Periodontitis cases Actinobacillus actinomycetumcomitans (AA) has also been found in the tissues. Bacteria may invade intercellular space under exfoliating epithelial cells but also found between deeper epithelial cells and accumulating on the basement lamina. Some bacterial traverse the basement lamina and invade the subepithelial connective tissue.
- 23. The micro topography of the gingival wall of the pocket SEM reveals several areas in the soft tissue wall of the pocket where different types of activity take place. These areas are irregularly oval or elongated and adjacent to one another and measure about 50-200 micrometer. This suggests that the pocket wall is the constantly changing as a result of interaction between host and bacteria. Following areas have been noted-: (a) Area of relative quiescence: Shows relatively flat surface with minor depressions & mounds and occasional shedding of cells. (b)Area of bacterial accumulation: which appear as depression on the epithelial surface with abundant debris and bacterial clumps penetrating into the enlarged intercellular spaces. These Bacteria are mailnly Rod, cocci, filamentous & a few spirochetes. (c) Areas of emergence of leukocyte: leucocyte appear in the pocket wall through holes located in the intercellular spaces. Scanning electron frontal micrograph of the periodontal pocket wall. Different areas can be seen in the pocket wall surface. A, Area of quiescence; B, bacterial accumulation; C, bacterial-leukocyte interaction; D, intense cellular desquamation. Arrows point to emerging leukocytes and holes left by leukocytes in the pocket wall. (×800.)
- 24. (d)Areas of Leukocyte-bacteria interaction: Numerous leukocytes are present & covered with bacteria in an apparent process of phagocytosis. Bacterial plaque associated with the epithelium is seen either as an organised matrix covered by a fibrin like material in contact with the surface of cells or as bacteria penetrating into the intercellular spaces. (e)Areas of intense epithelial desquamation: consist of semi- attached & folded epithelial squames, sometimes partially covered with bacteria. (f)Areas of ulcerations with exposed connective tissue. (g)Areas of haemorrhage with numerous erythrocytes. Note the desquamating epithelial cells and leukocytes (white arrows) emerging onto the pocket space. Scattered bacteria can also be seen (black arrow)
- 25. The transition from one area to another could result from: Bacterial accumulation in previously quiescent areas ↓ Triggering the emergence of leukocytes ↓ Leukocyte-bacteria interaction ↓ Lead to intense Epithelial desquamation ↓ Finally to ulceration & haemorrhage
- 26. PERIODONTAL POCKET AS A HEALING LESIONS Periodontal pocket are chronic inflammatory lesion and thus constantly undergoing repair. Complete healing does not occur because of persistence of the bacterial attack which continues to stimulate an inflammatory response, causing degeneration of the new tissues formed in continuous effort at repair. There are destructive and constructive tissue changes and their balance determines the clinical features as color, consistency & surface texture of the pocket wall. If Inflammatory fluid & cellular exudate predominate, the pocket wall is bluish-red, soft, spongy and friable, with a smooth, shiny surface, at the clinical level and this is referred to as an edematous pocket wall.
- 27. If there is predominance of newly formed connective tissue cells & fibers, the pocket wall is more firms and pink, and known as fibrotic pocket wall. Edematous and fibrotic pockets represent opposite extremes of the same Pathologic process, not different disease entities. Fibrotic pocket walls may be misleading because they do not necessarily reflect what is taking place throughout the pocket wall. The most severe degenerative changes in periodontal tissues occur adjacent to the tooth surface & subgingival plaque. In some cases inflammation and ulceration on inside of the pocket are walled off by fibrous tissue on the outer aspects. Externally the pocket appears pink and fibrotic, despite the inflammatory changes occurring internally.
- 28. POCKET CONTENT Periodontal pocket contains – Debris (consisting of microorganism & their products mainly enzymes, endotoxins and other metabolic product) Gingival fluid Food remnants Salivary mucin Desquamated epithelial cells & Leukocytes Plaque covered calculus projects from tooth surface. If purulent exudate present:consists of– Living, degenerated and necrotic leukocytes, Living and dead bacteria Serum A scant amount of fibrin.
- 29. Significance Of Pus Formation Pus is common feature of periodontal diseases, but it is only a secondary sign. The presence of pus or ease with which it can be expressed from the pocket merely reflects nature of the inflammatory changes in the pocket wall. It is not an indication of the depth of the pocket or the severity of the destruction of the supporting tissues. Extensive pus formation may occur in shallow pockets whereas deep pockets may exhibit little or no pus.
- 30. ROOT SURFACE WALL The root surface wall of periodontal pocket often undergoes changes that are significant because they may perpetuate the periodontal infection, causing pain, and complicate periodontal treatment. As the pocket deepens, collagen fibers embedded in the cementum are destroyed ↓ Cementum become exposed to the oral environment ↓ Remanents of Sharpey’s fibers in the cementum undergo degeneration ↓ Creating a favorable environment for bacterial penetration ↓ Penetration and growth of bacteria leads to fragmentation and breakdown of the cementum surface ↓ Result in area of necrotic cementum, separated from the tooth by mass of bacteria
- 31. Decalcification And Remineralisation Of Cementum Areas of increased mineralization: Probably a result of an exchange, on exposure to the oral cavity, of minerals and organic components at the cementum- saliva interface. The mineral content of exposed cementum increases. The minerals that are increased in diseased root surfaces include Ca, Mg, P & F. Micro hardness, however, remains unchanged. The development of highly mineralized superficial layer may increase the tooth resistance to decay. Areas of demineralization/Root carries: Exposure to oral fluid and bacterial plaque results in proteolysis of the embedded remnants of the Sharpy's fibres. The cementum may be softened & may undergo fragmentation and cavitations. Unlike Enamel caries, root surface caries tend to progress around rather that into the tooth.
- 32. Active well defined yellowish/ Light brown areas frequently covered by plaque have softened or leathery consistency on probing Inactive well defined darken lesion with a smooth surface harder consistency on probing Root caries lesion Caries of the cementum require special attention when the pocket is treated. The necrotic cementum must be removed by scaling and root planing until firm tooth surface is reached even if this extended in dentin
- 33. Areas of cellular resorption of cementum and dentin They are common in roots unexposed by periodontal diseases. They are of no significance because they are symptom free and as along as the root is covered by the periodontal ligament, they are likely to undergo repair.
- 34. Surface Morphology Of Tooth Wall Of Periodontal Pocket The following zones can be found in the bottom of a periodontal pocket: 1. Cementum covered by calculus 2. Attached Plaque – covers calculus and extends apically from it to a variable degree (100-500 m) 3. The zone of unattached plaque Surround attached plaque & extends apically to it. 4. The zone of attachment of Junctional Epithelium to the tooth – this zone reduced to 100 m (in periodontal pocket) from 500 m found in normal sulcus. 5. a zone of semi-destroyed connective tissue fibres – apical to the JE
- 35. PERIODONTAL DISEASE ACTIVITY According to the concept of periodontal disease activity, periodontal pockets go through - 1. PERIODS OF QUIESCENCE OR INACTIVITY Characterized by a reduced inflammatory response & little or no loss of bone and connective tissue attachment. A build up of unattached plaque with its gram-negative, motile and anaerobic bacteria. 2. PERIODS OF EXACERBATION OR ACTIVITY Bone and connective tissue attachment are lost and the pocket deepens. This period may lasts for days, weeks, months & eventually followed by a period of remission or quiescence in which G+ve bacteria proliferate and a more stable condition is established. Clinical features: shows bleeding spontaneous or on probing and greater amount of gingival exudates. Histological Features : Pocket Epithelium appears thin and ulcerated, Infiltrate composed of plasma cells & PMN leukocytes.
- 36. SITE SPECIFICITY Periodontal destruction does not occur in all parts of the mouth at the same time but rather on a few teeth at a time or even only some aspects of some teeth at any given time. This is referred to as the site specificity of the periodontal disease.
- 37. PULP CHANGES ASSOCIATED WITH PERIODONTAL POCKET Spread of infection from periodontal pockets may cause pathologic changes to the pulp. It may give rise to painful symptoms. Involvement of the pulp may occure through either the apical foramen or the lateral canals. Atrophic and inflammatory pulpal changes may occur in such cases.
- 38. RELATION OF ATTACHMENT LOSS & BONE LOSS TO POCKET DEPTH Pocket formation leads to loss of attachment of gingiva & denudation of root surface. The severity of attachment and bone loss is generally correlated with the depth of the pocket. The degree of attachment loss depends on the location of base of pocket on the root surface. Whereas pocket depth is the distance between the base of the pocket & the crest of the gingival margin. Excessive attachment & bone loss may be associated with shallow pocket if the attachment loss is accompanied by recession of gingival margin, and slight bone loss can occur with deep pockets.
- 39. AREA BETWEEN THE BASE OF THE POCKET AND ALVELOR BONE Normally the distance between the apical end of the Junctional epithelium & alveolar bone is relatively constant. The distance between apical extent of calculus & alveolar crest in periodontal pocket is most constant and has 1.97mm (± 33.16%) The distance from attached plaque to bone is never less than 0.5 mm and never more than 2.7 mm. These findings suggest that the bone resorbing activity induced by bacteria is exerted within these distances.
- 40. RELATIONSHIP OF PERIODONTAL POCKET TO BONE: INTRABONY POCKET Base of the pocket is apical to the crest of alveolar bone, and the pocket wall lies b/w the tooth and the bone. Mostly occur interproximally but may be located on facial and lingual tooth surfaces. The bone destructive pattern is vertical/Angular. On facial and lingual surface, the periodontal fibres follow angular pattern of adjacent bone. SUPRABONY POCKET Base of pocket is coronal to the level of alveolar bone. Pattern of destruction of underlying bone is horizontal. The transseptal fibers are arranged horizontal in space between base & alveolar bone. On the facial and lingual surface, PDL fibers beneath pocket follow their normal horizontal-oblique pattern.
- 41. Radiographic and Microscopic features of intrabony pockets
- 42. “ A periodontal abscess is a localized purulent inflammation in the periodontal tissue” It is also k/a lateral abscess or parietal abscess. “abscess localized in gingiva, caused by injury to the outer surface of the gingiva, and not involving the supporting structure are called gingival abscesses” Periodontal abscess on an upper right central incisor.
- 43. Periodontal abscess formation may occur in the following ways: 1. Extension of infection from a periodontal pocket deeply into the supporting periodontal tissues and localization of the suppurative inflammatory process along the lateral aspect of the root. 2. Lateral extension of inflammation from the inner surface of a periodontal pocket into the connective tissue of the pocket wall. Formation of the abscess results when drainage into the pocket space is impaired. 3. Formation in a pocket with a tortuous course around the root. A periodontal abscess may form in the cul-de-sac, the deep end of which is shut off from the surface. 4. Incomplete removal of calculus during treatment of a periodontal pocket. The gingival wall shrinks, occluding the pocket orifice, and a periodontal abscess occurs in the sealed-off portion of the pocket. 5. After trauma to the tooth or with perforation of the lateral wall of the root in endodontic therapy. In these situations, a periodontal abscess may occur in the absence of periodontal disease.
- 44. Periodontal abscesses are classified according to location as follows: 1. Abscess in the supporting periodontal tissues along the lateral aspect of the root. In this condition, a sinus generally occurs in the bone that extends laterally from the abscess to the external surface. 2. Abscess in the soft tissue wall of a deep periodontal pocket.
- 45. The localized acute abscess becomes a chronic abscess when its purulent content drains through a fistula into the outer gingival surface or into the periodontal pocket and the infection causing the abscess is not resolved. Microscopic view of a periodontal abscess showing dense accumulation of polymorphonuclear leukocytes (PMNs) covered by squamous epithelium. Microscopically, an abscess is a localized accumulation of viable and nonviable PMNs within the periodontal pocket wall. The PMNs liberate enzymes that digest the cells and other tissue structures, forming the liquid product known as pus, which constitutes the center of the abscess. An acute inflammatory reaction surrounds the purulent area, and the overlying epithelium exhibits intracellular and extracellular edema and invasion of leukocytes.
- 46. The periodontal cyst is an uncommon lesion that produces localized destruction of the periodontal tissues along a lateral root surface, most often in the mandibular canine-premolar area. It is considered to be derived from rests of Malassez or other proliferating odontogenic rests. A periodontal cyst is usually asymptomatic, without grossly detectable changes, but it may present as a localized, tender swelling.
- 47. Radiographically, an interproximal periodontal cyst appears on the side of the root as a radiolucent area bordered by a radiopaque line. Its radiographic appearance cannot be differentiated from that of a periodontal abscess. Microscopically, the cystic lining may be 1. A loosely arranged, thin, nonkeratinized, epithelium, sometimes with thicker proliferating areas or 2. An odontogenic keratocyst.
