The document provides a comprehensive overview of gingival recession, including definitions, classifications, etiology, and treatment options. It discusses various classifications of gingival recession, limitations of current classifications, and multiple factors contributing to its occurrence. Additionally, it highlights the prevalence of gingival recession in different populations and its implications for dental health.
![ Gingival recession: Defined as a situation where the gingival margin
lies against any part of the root surface of the tooth. It usually implies
recession affecting the facial aspect of a root. (Smith R G, 1997)
Gingival recession is defined as the apical migration of the junctional
epithelium with exposure of root surfaces.[Kassab MM, Cohen RE-
2003].](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-6-320.jpg)

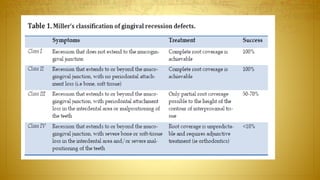
![Miller has primarily based his classification of gingival recession defects
on two aspects:
[1] Extent of gingival recession defects and
[2] Extent of hard and soft tissue loss in interdental areas
surrounding the gingival recession defects.](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-15-320.jpg)




![ANATOMICAL FACTORS
.
One etiologic factor that may be associated
with gingival recession is a prior lack of
alveolar bone at the site [Watson PJ-
1984].](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-48-320.jpg)
![PHYSIOLOGICAL FACTORS
Orthodontic movement of teeth to
positions outside the labial or lingual
alveolar plate, leading to dehiscence
formation.
[Wennström JL, Lindhe J, Sinclair F,
Thilander B-1987].](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-49-320.jpg)
![ Traumatic mechanical tooth brushing is a factor in the etiology of gingival
recession. Recession due to tooth brushing was characteristically
localized on facial surfaces and frequently “V” shaped, often occurring in
association with tooth abrasion. [Gillette WB, Van house RL.-1980]
Epidemiologic studies have supported the idea that traumatic tooth
brushing may be associated with gingival recession, with buccal gingival
recession noted more frequently on the left side of the jaw. [Addy M,
Mostafa P, Newcombe RG-1987].](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-53-320.jpg)
![ABERRANT FRENAL ATTACHMENT
Some studies did not find any correlation between frenal pull and recession
[Trott JR, Love B-1966] whereas others did find an association [Parfitt GJ,
Mjor JA-1964].](https://image.slidesharecdn.com/recession-200526140606/85/Gingival-Recession-54-320.jpg)