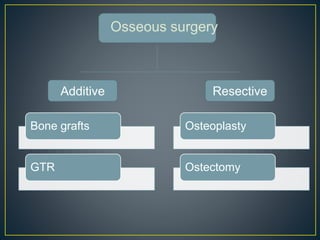
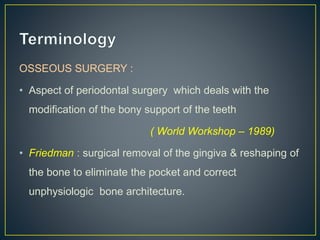
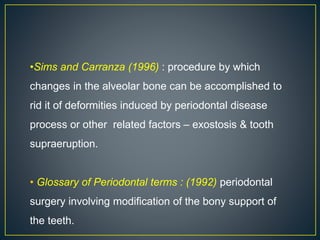
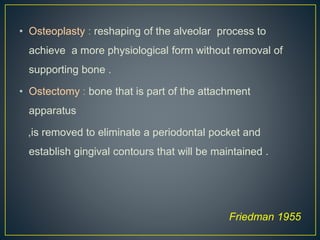
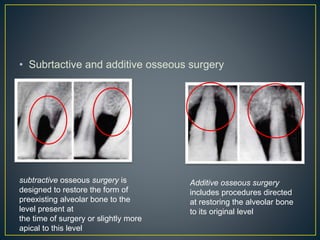
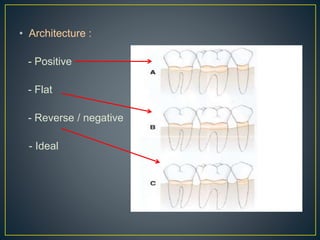
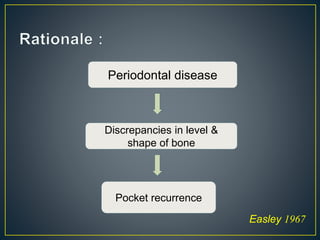
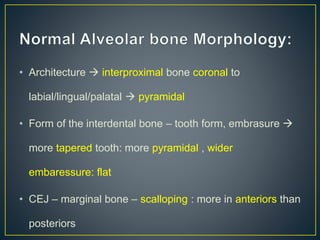
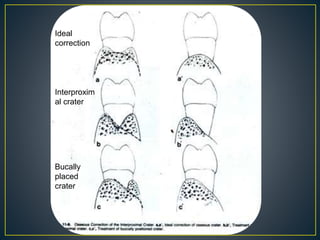
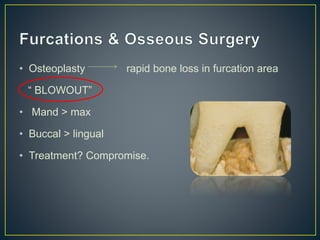
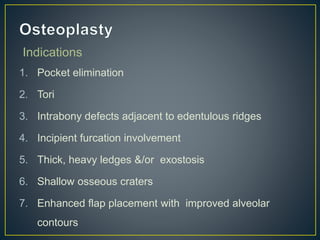
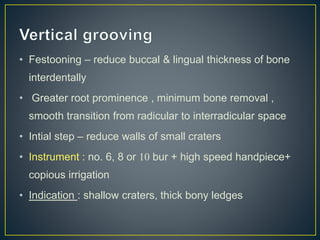
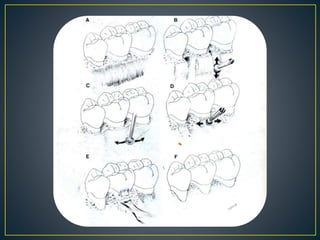
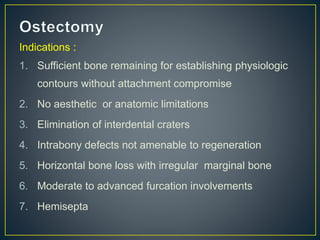
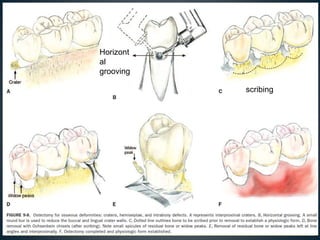
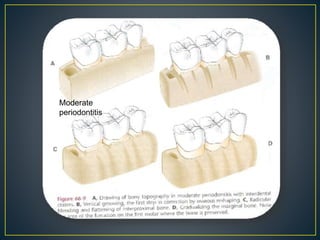
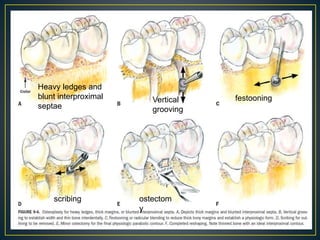
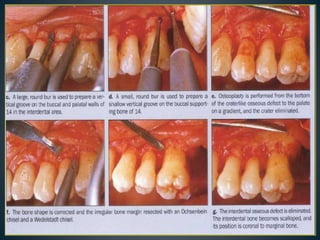
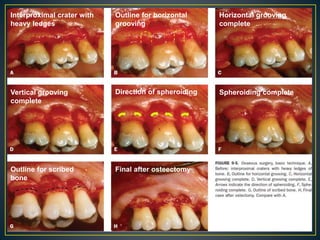
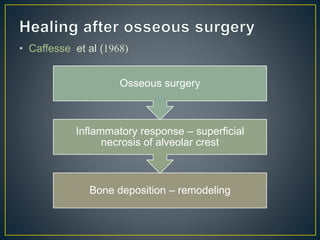
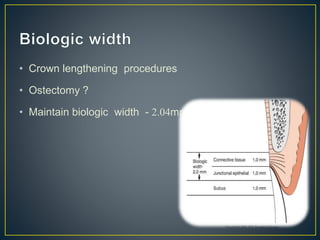
1. Osseous surgery involves modifying the alveolar bone support of teeth and includes techniques like osteoplasty and ostectomy. It aims to eliminate pockets and correct unphysiological bone architecture.
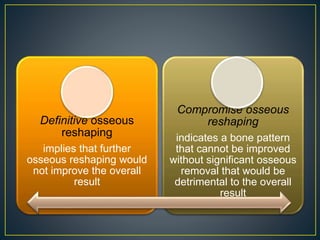
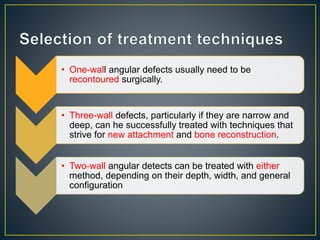
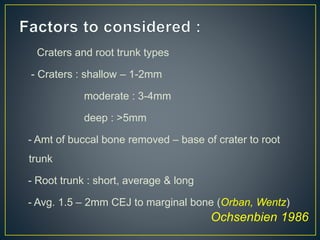
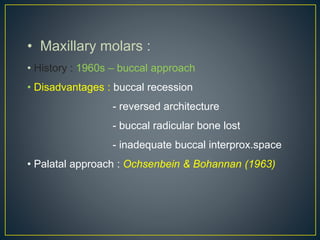
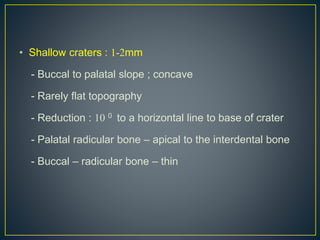
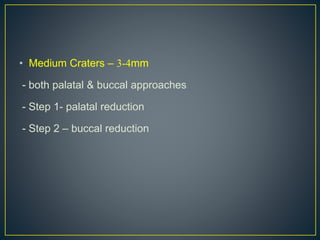
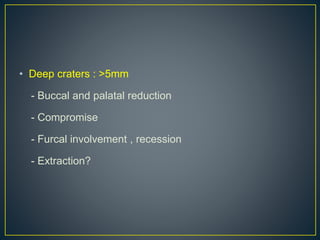
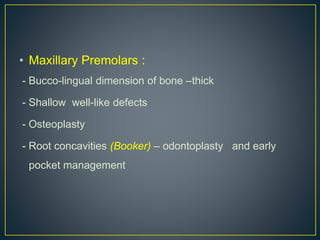
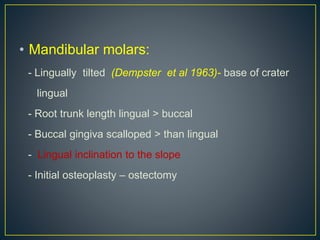
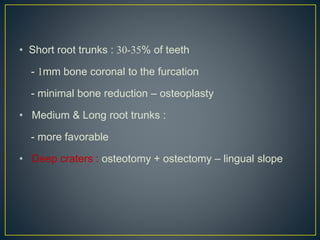
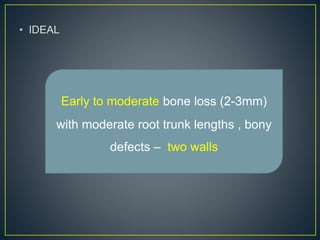
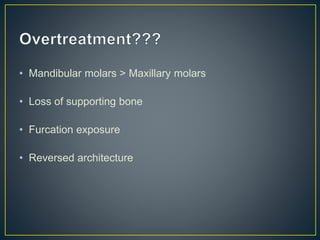
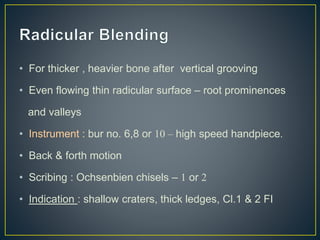
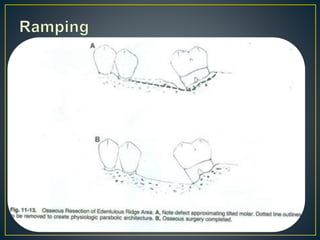
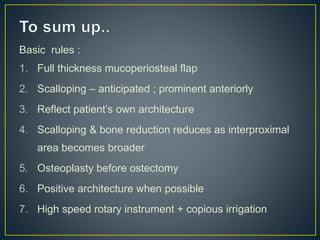
2. Factors in selecting a technique include the amount and location of bone loss, root trunk length, and anatomical limitations. Techniques range from non-resective procedures like osteoplasty to resective procedures like ostectomy.
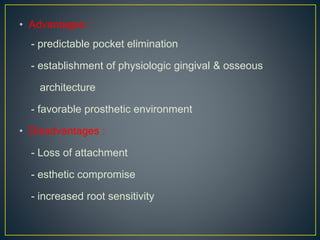
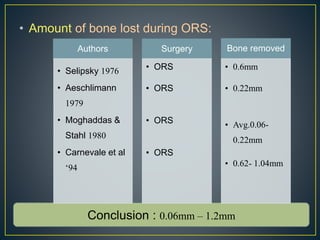
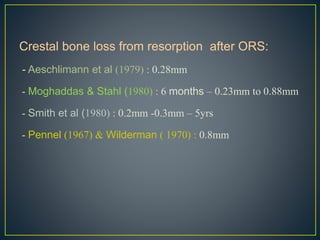
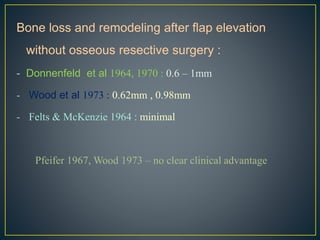
3. Outcomes of osseous surgery generally include pocket elimination and establishment of physiological bone contours and architecture, though some bone loss from remodeling is expected in the range of 0.06mm to 1.2mm.