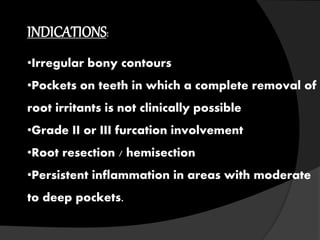
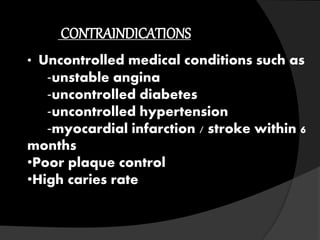
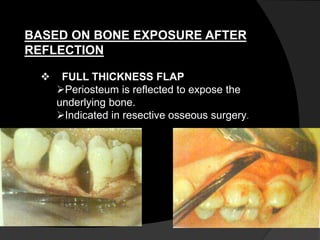
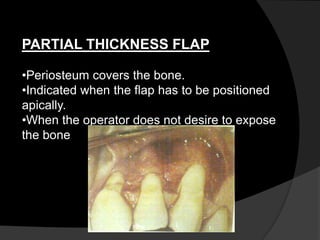
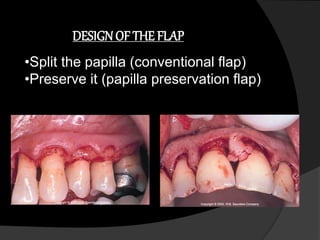
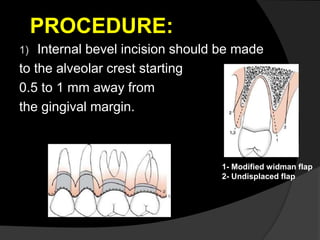
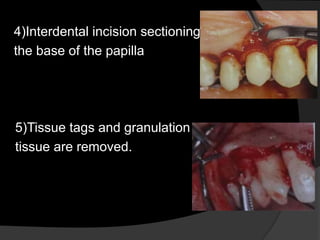
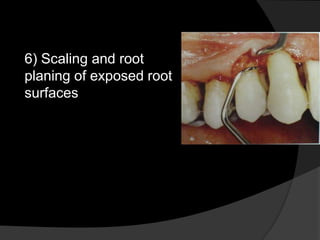
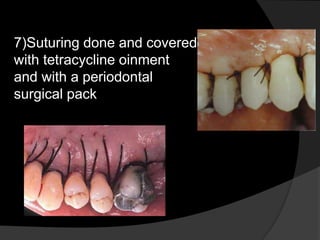
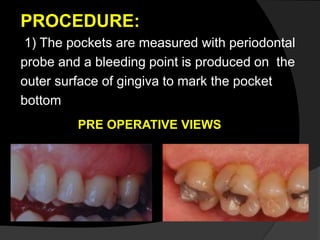
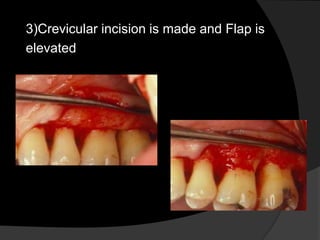
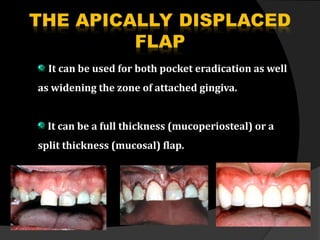
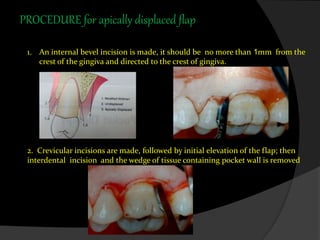
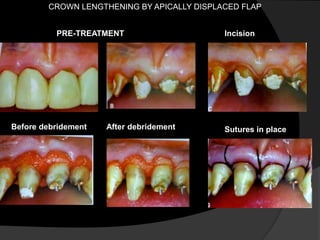
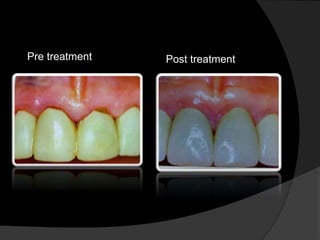
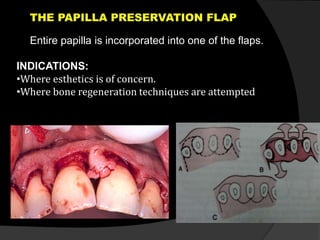
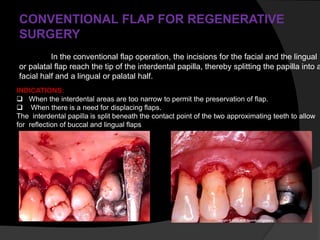
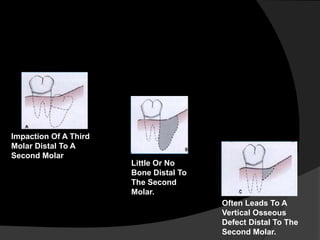
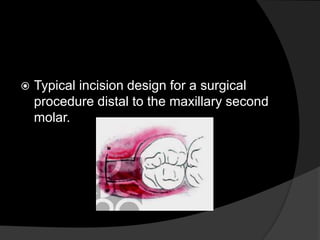
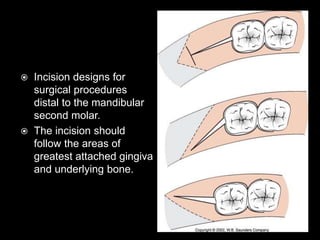
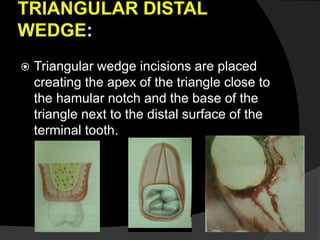
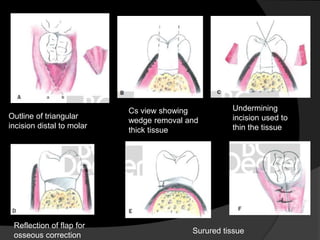
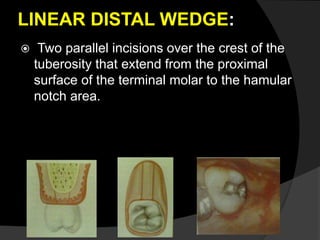
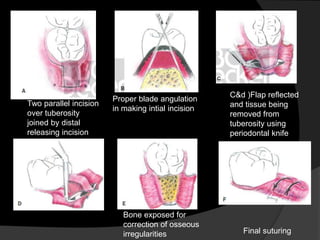
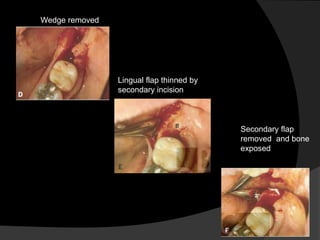
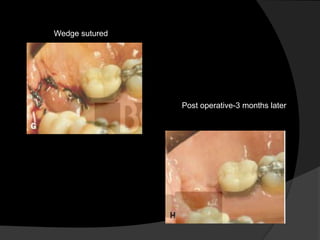
This document discusses different types of periodontal flaps used in periodontal surgery. It defines a periodontal flap as a section of gingiva and/or mucosa surgically separated from underlying tissues to provide access to bone and roots. It describes various classifications of flaps based on bone exposure, flap placement, papilla management, and indications for specific flap types like modified Widman flap and apically displaced flap. Distal molar surgery flaps like triangular and linear wedge designs are also summarized. The document provides detailed procedures and pre/post operative views for different flap techniques.