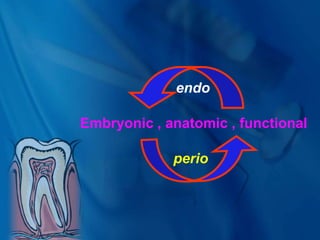
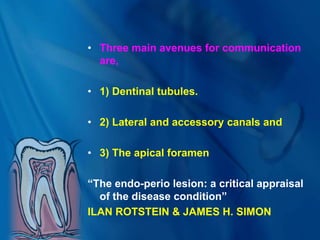
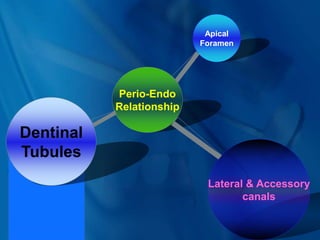
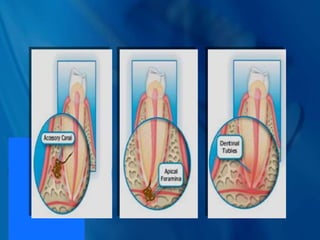
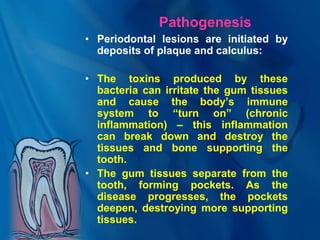
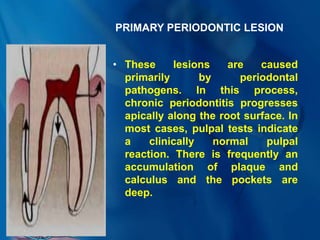
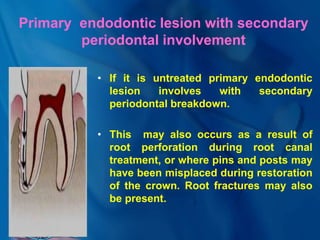
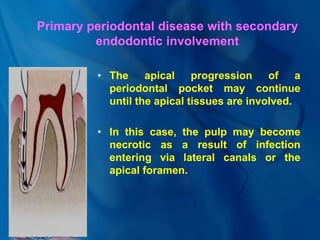
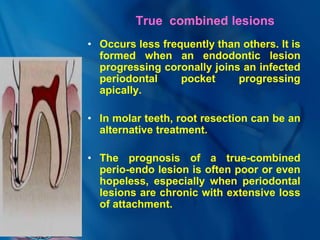
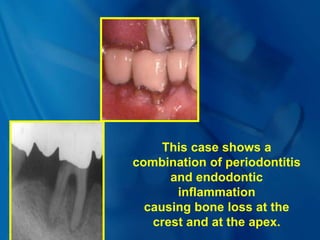
1) Endo-perio lesions occur when inflammation and infection spreads between the pulp and periodontium. There are three main pathways of communication: dentinal tubules, lateral/accessory canals, and the apical foramen.
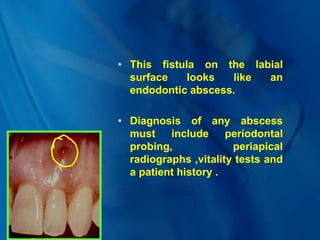
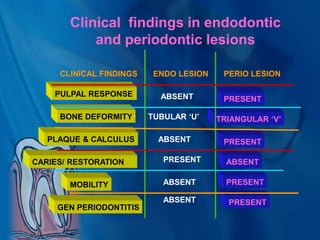
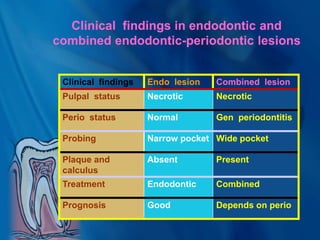
2) Diagnosing endo-perio lesions can be complicated, as they involve both pulp and periodontal components. Clinical findings, radiographs, vitality tests, and probing are used.
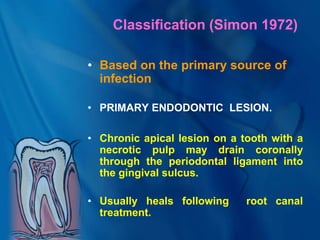
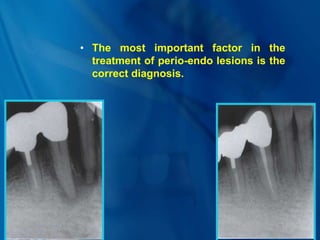
3) Treatment depends on whether the primary source of infection is endodontic, periodontal, or both. It may involve endodontic therapy, periodontal therapy, or a combined approach. Correct diagnosis is important for determining the proper treatment plan.