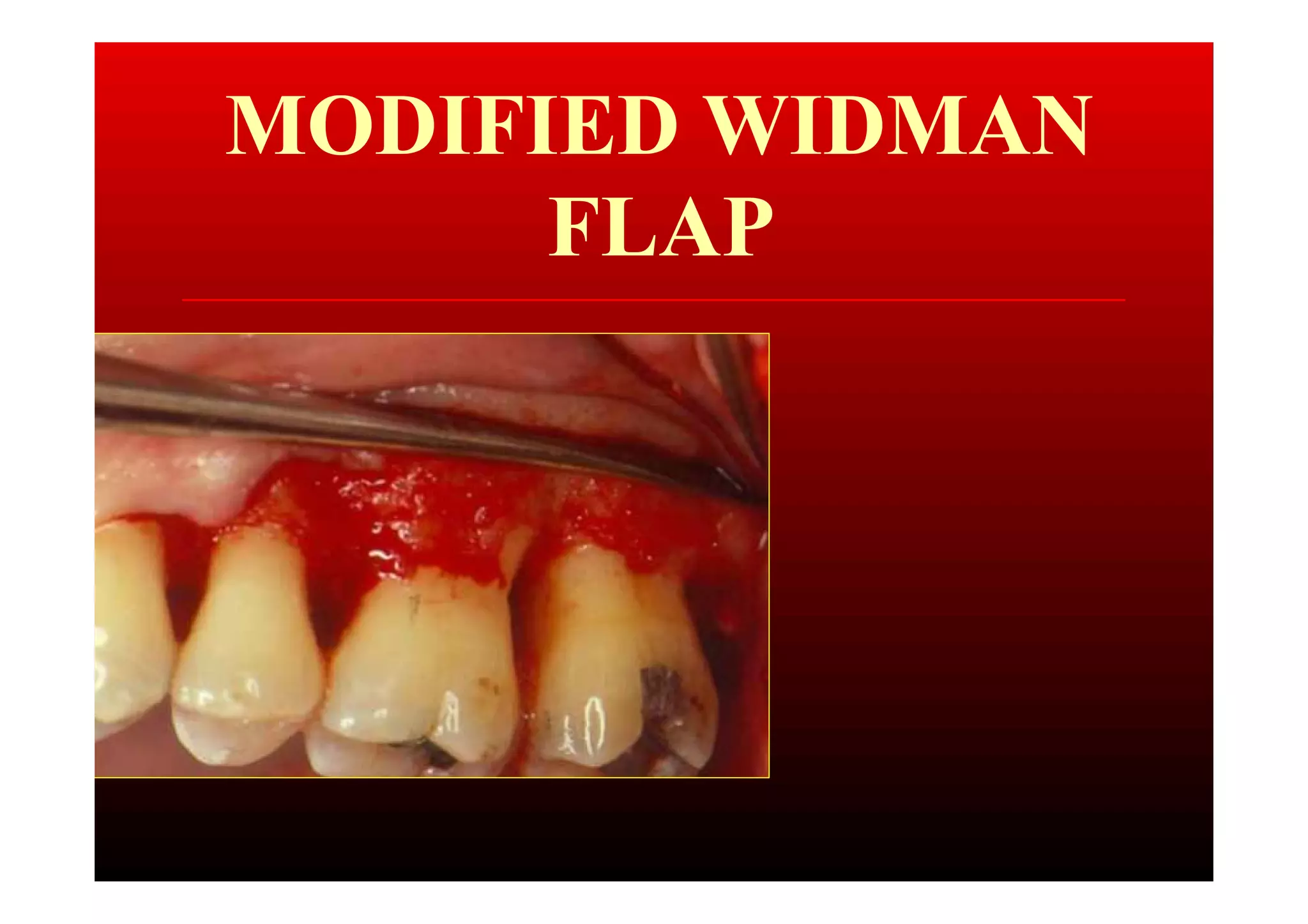
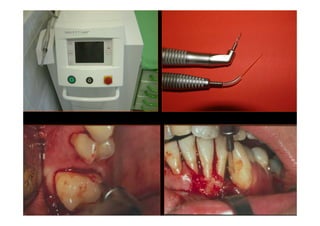
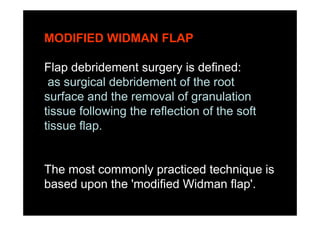
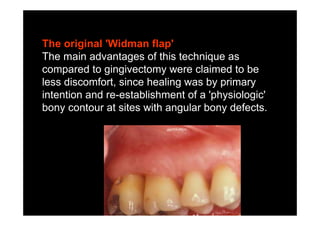
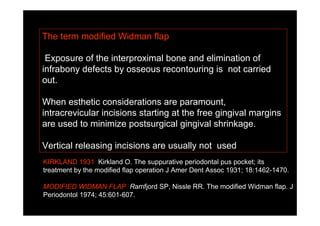
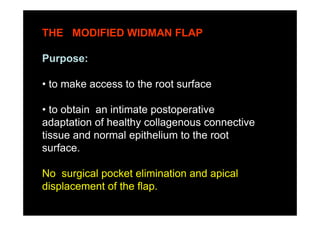
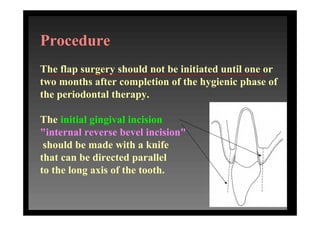
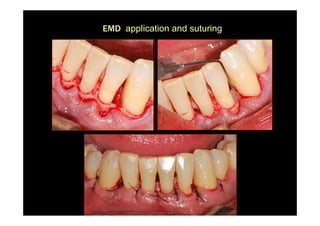
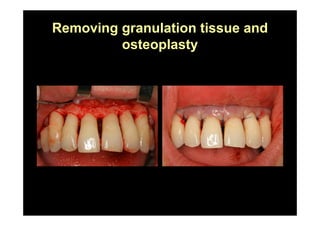
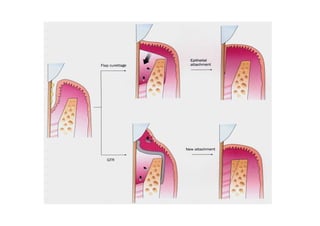
The modified Widman flap is a periodontal surgical technique used to obtain access to the root surface and allow for intimate postoperative adaptation of healthy connective tissue and epithelium to the root surface. Key aspects include:
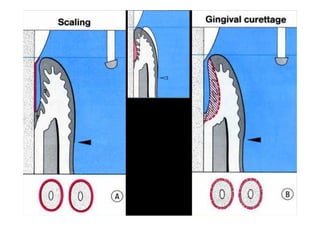
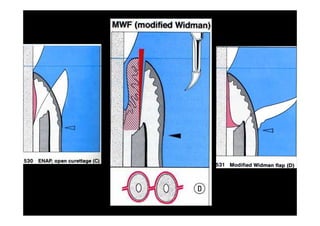
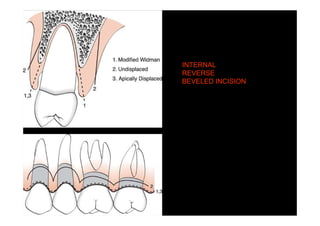
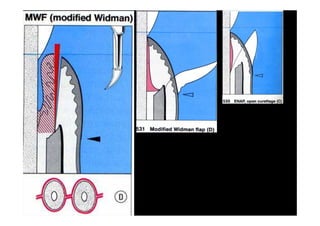
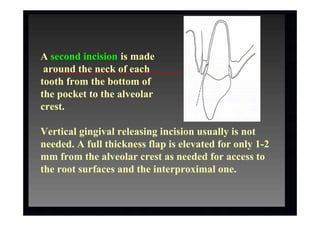
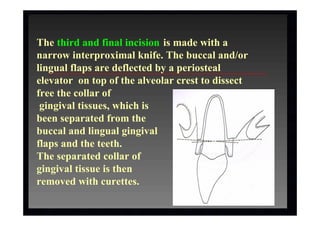
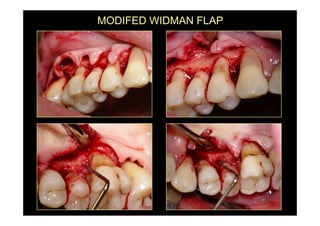
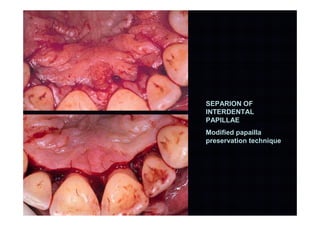
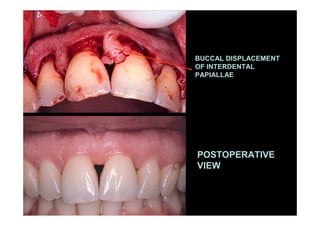
1. Incisions are made internally and intracrevicularly to minimize tissue loss and gingival shrinkage. Vertical releasing incisions are usually not used.
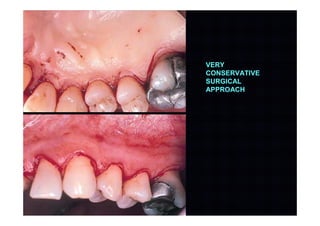
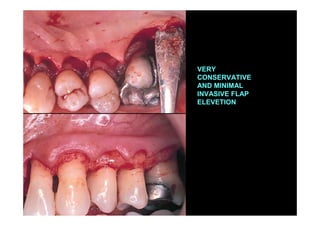
2. The goal is access for root debridement rather than pocket elimination. Minimal flap elevation of 1-2mm is done to access root surfaces.
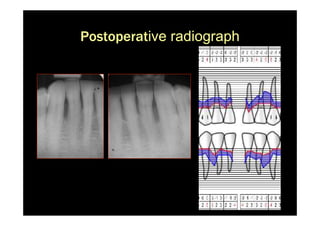
3. It is indicated for mild to moderate periodontitis with pocket depths up to 6mm and minimal inflammation. Primary intention healing occurs.