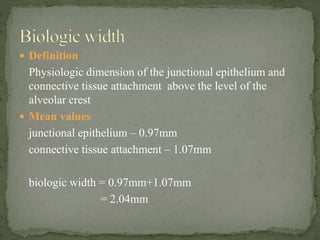
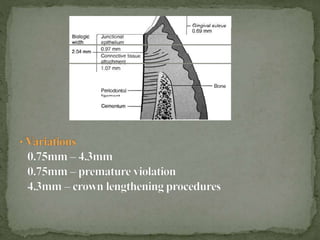
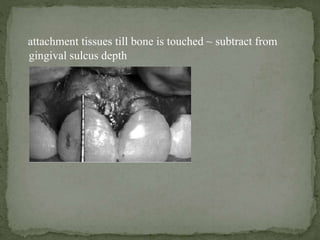
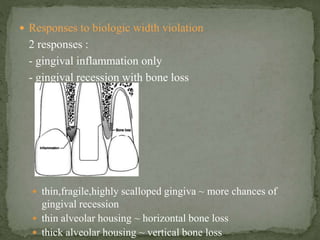
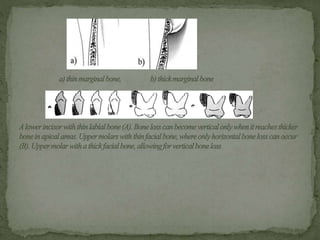
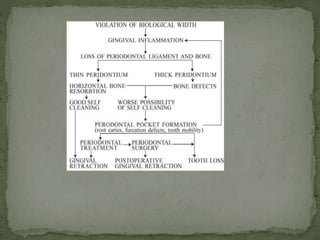
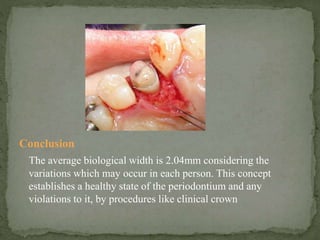
The biological width refers to the dimensions of the junctional epithelium and connective tissue attachment above the alveolar crest, which averages 2.04mm. Placement of restoration margins within 1mm of the gingival sulcus is ideal to preserve this biological width, while subgingival placement can lead to inflammation, recession, or bone loss by violating the biological width. When a violation occurs, it can be corrected by surgery to remove bone away from the margin by the ideal biological width distance, or by orthodontic extrusion. Maintaining the biological width is essential for periodontal health.