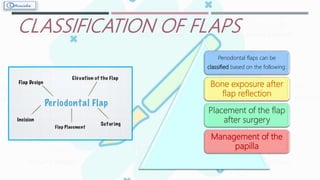
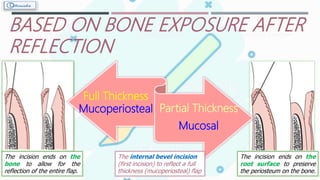
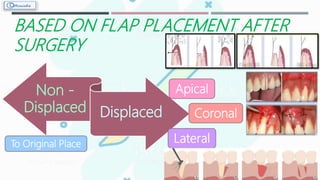
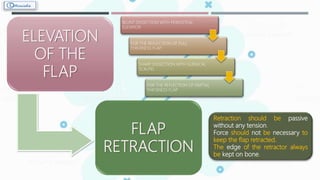
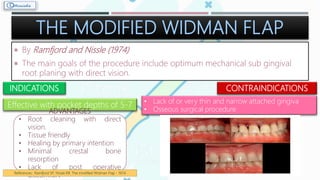
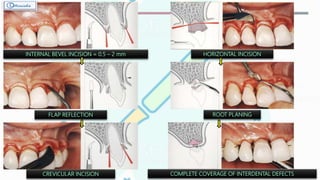
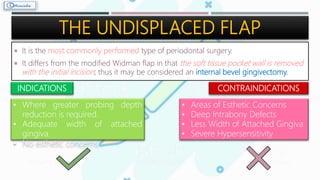
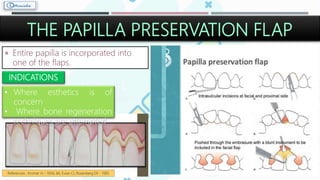
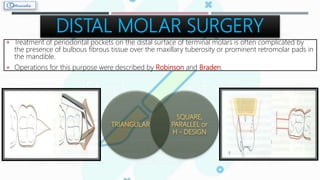
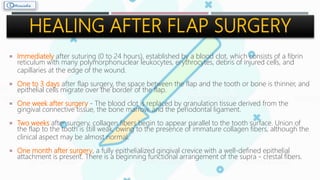
A periodontal flap is a section of gingiva and/or mucosa surgically separated from underlying tissues to provide visibility and access to the bone and root surface. It allows cleaning of root surfaces and treatment of bony irregularities to reduce pockets, infections, and inflammation. Flaps are classified based on bone exposure, placement after surgery, and papilla management. Techniques include the conventional flap, modified Widman flap, papilla preservation flap, and apically displaced flap. Healing after flap surgery involves blood clot formation, granulation tissue development, collagen formation, and epithelial attachment within 1 month.