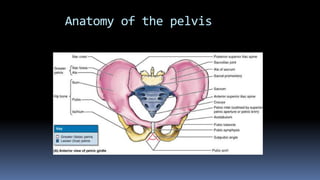
This document discusses the anatomy and classification of pelvic fractures. It begins by describing the bones that make up the pelvic ring - the innominate bones and sacrum. It then discusses the ligaments of the pelvic girdle and introduces different classifications of pelvic fractures including stable vs unstable fractures. The document goes on to describe specific fracture types under the Pennal and Tile classification including open book fractures. It discusses associated injuries from pelvic fractures like hemorrhage, neurologic and visceral injuries. Management of pelvic fractures is also summarized including initial stabilization, reduction techniques, complications and post-operative care.

















































![minor fracture [ stable ]
bed rest,
Painkiller
Physical therapy
Healing take 8-21 wk](https://image.slidesharecdn.com/anatomyofpelvis-150405123222-conversion-gate01/85/pelvis-finjury-51-320.jpg)











