This document discusses pelvic fractures, including:
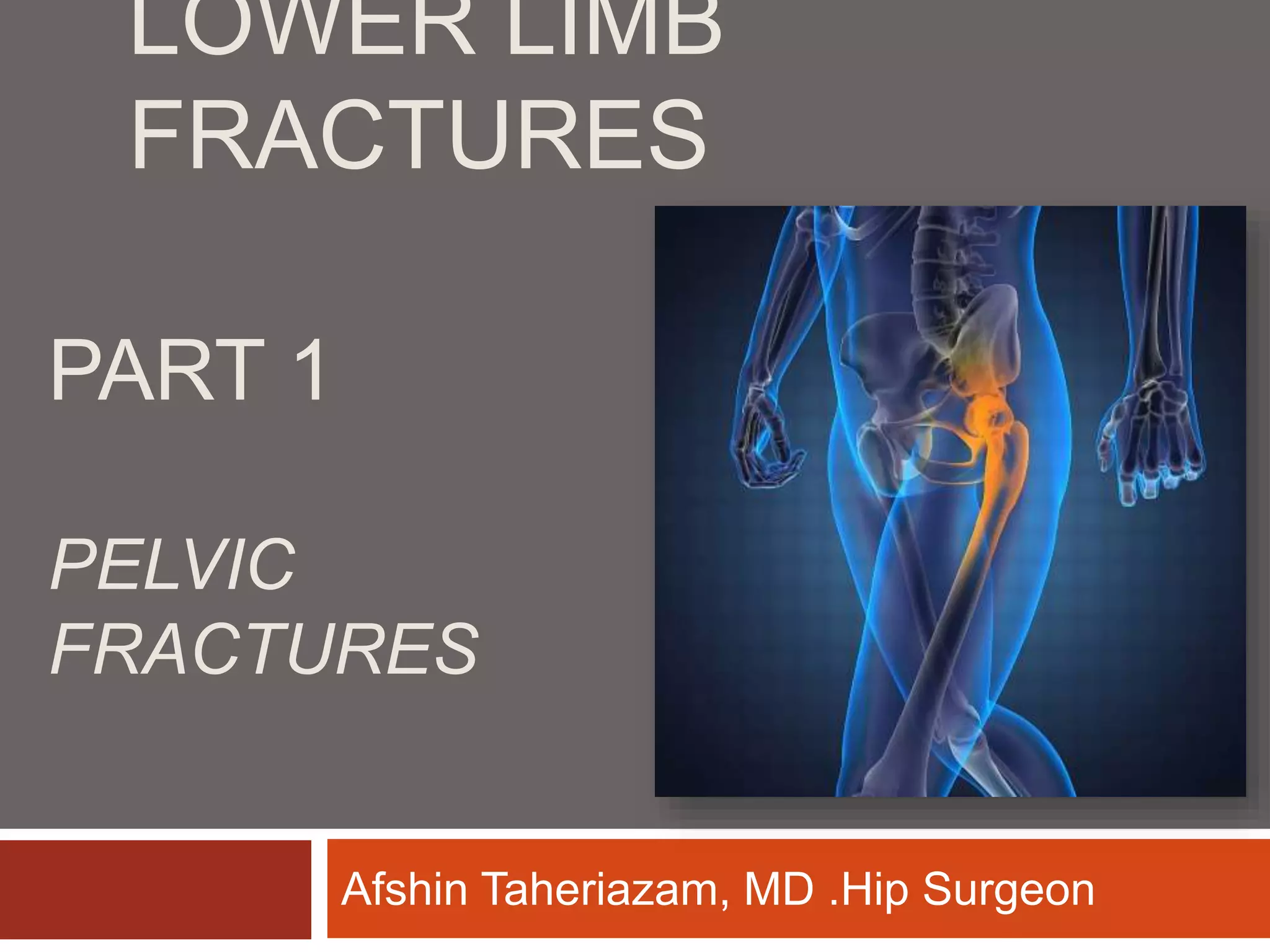
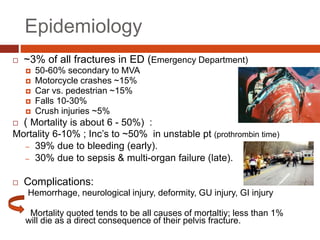
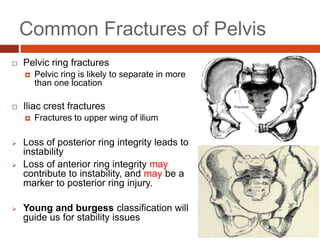
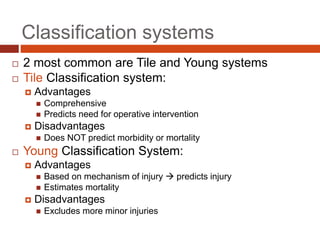
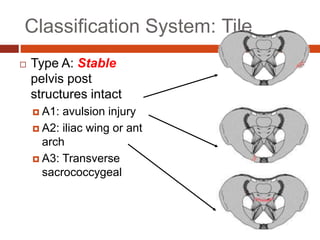
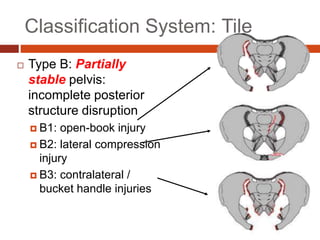
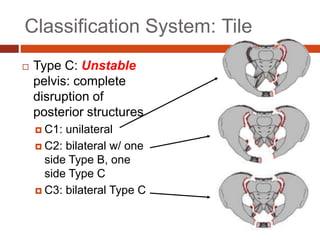
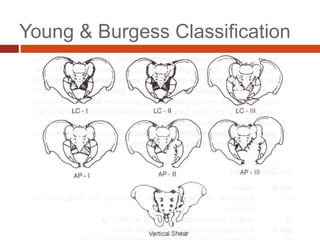
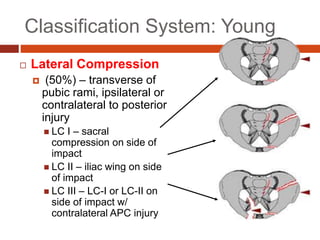
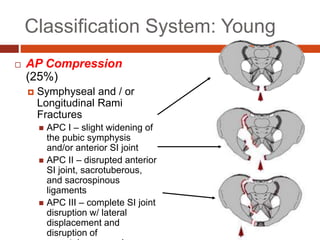
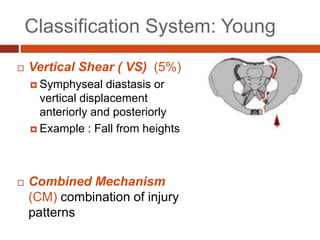
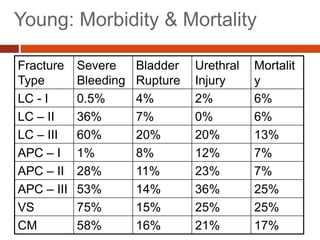
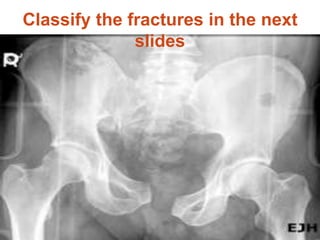
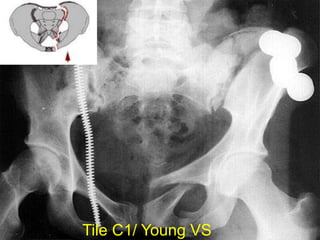
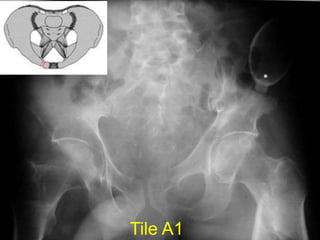
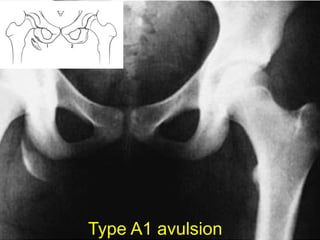
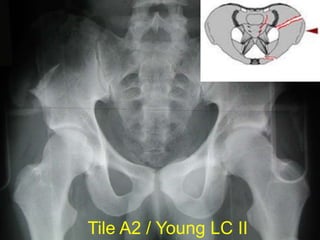
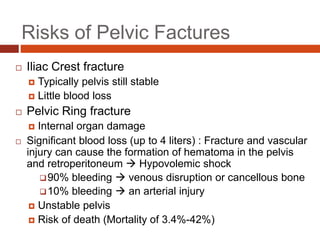
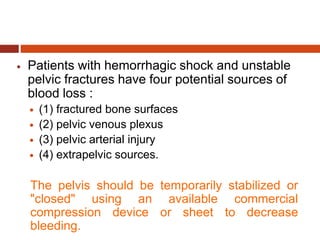
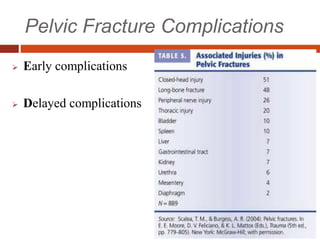
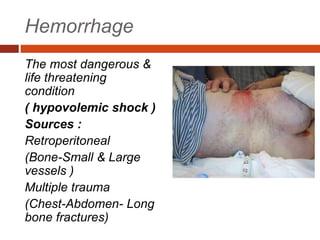
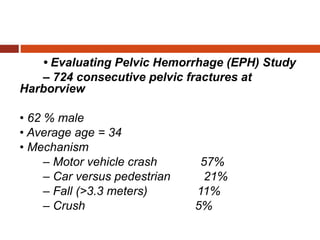
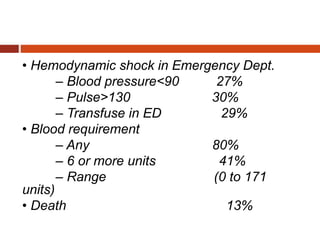
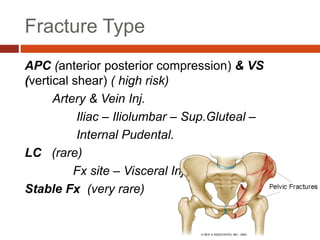
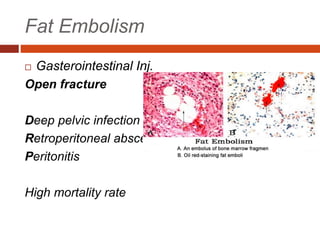
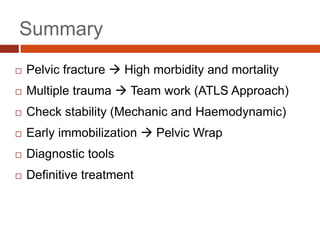
1. Epidemiology of pelvic fractures, their classification systems including Tile and Young & Burgess, and risks including significant blood loss.
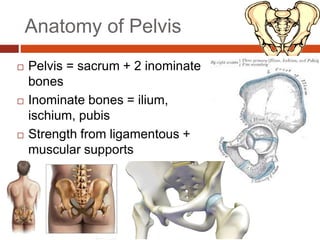
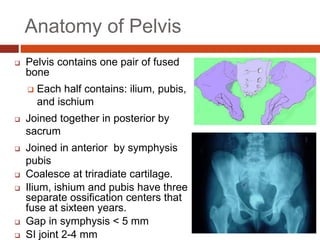
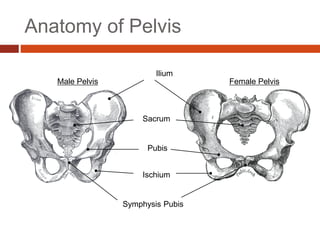
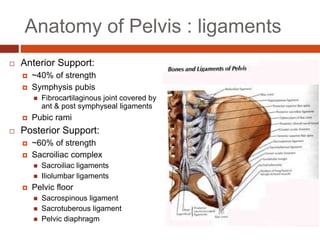
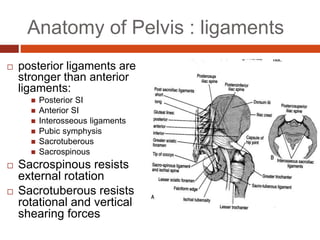
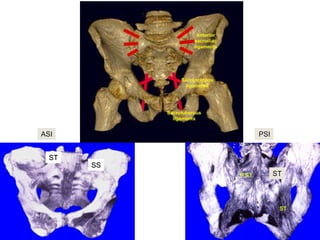
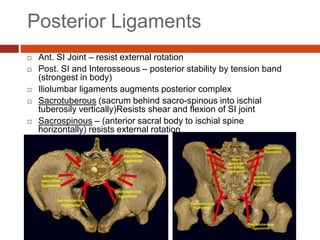
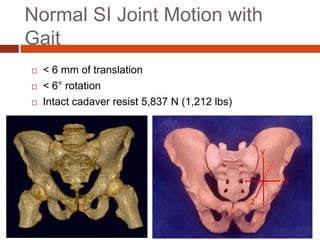
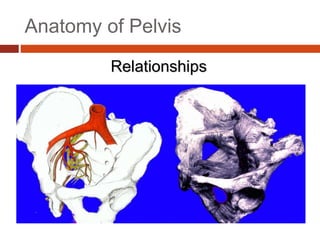
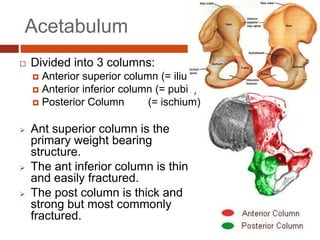
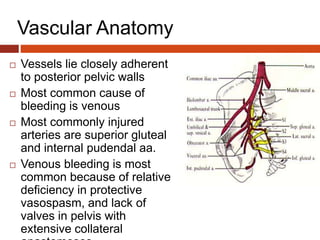
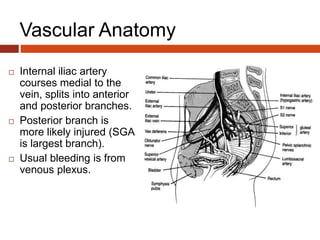
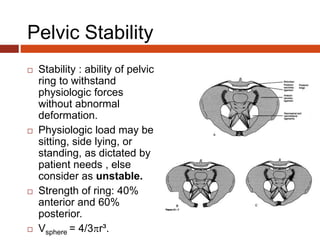
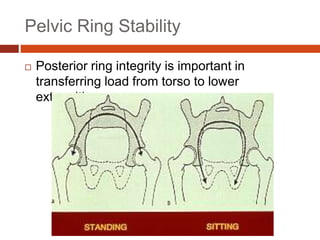
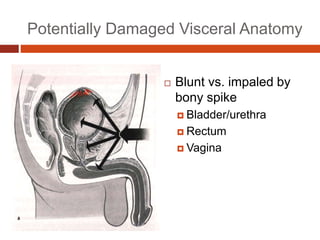
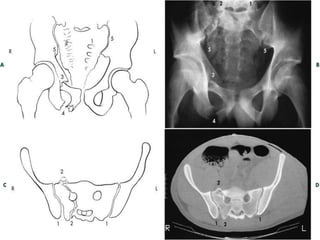
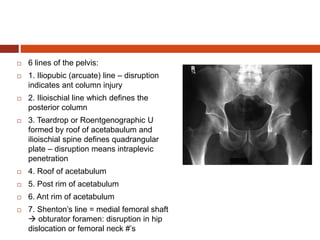
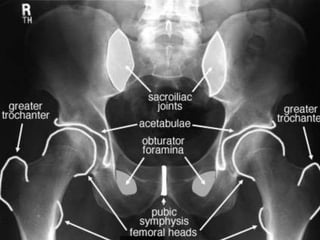
2. Anatomy of the pelvis including ligamentous supports, vascular structures, and relationships to other bones.
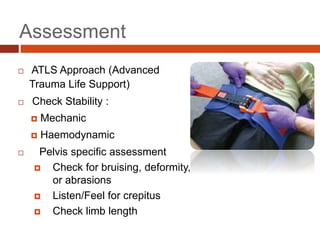
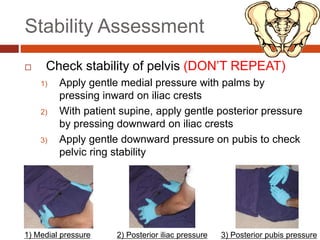
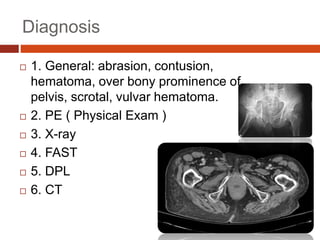
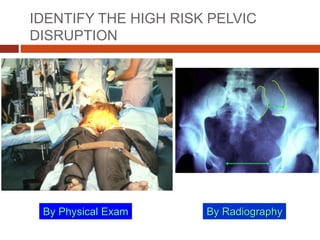
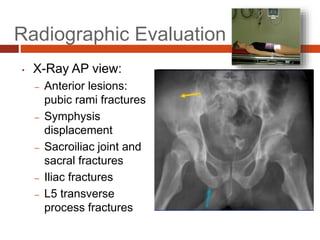
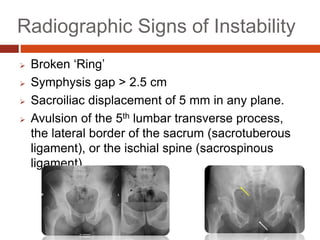
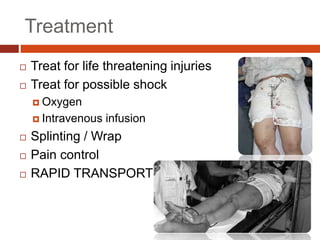
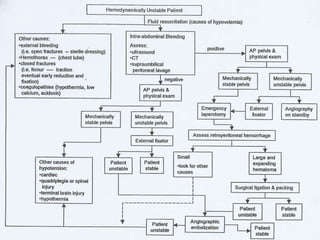
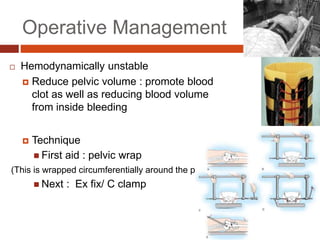
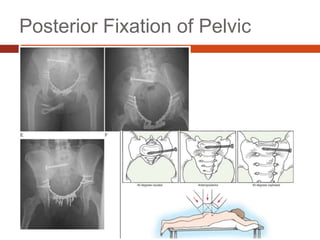
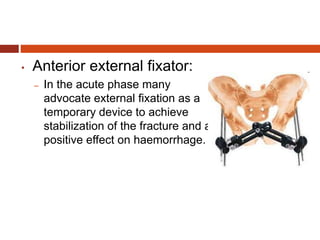
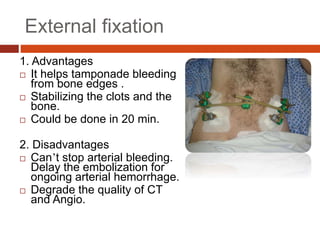
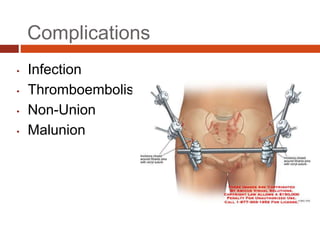
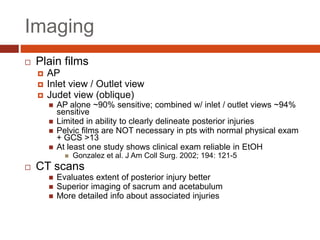
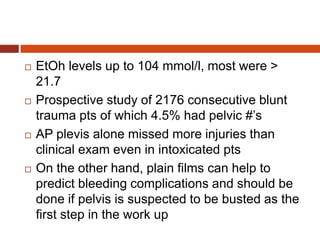
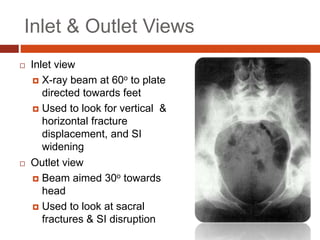
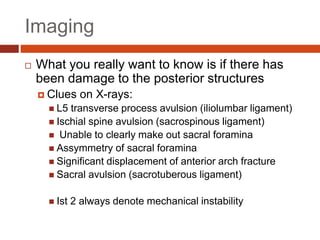
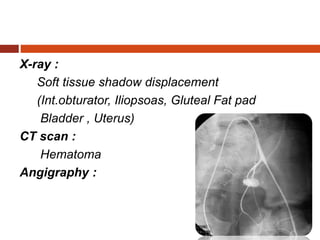
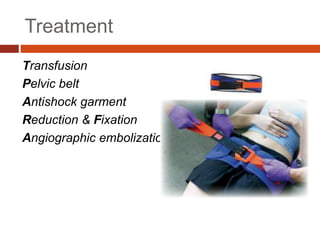
3. Assessment of pelvic fractures including checking stability and diagnostic imaging. Treatment may involve splinting and stabilization or surgery depending on stability and patient condition.