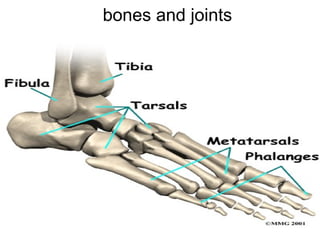
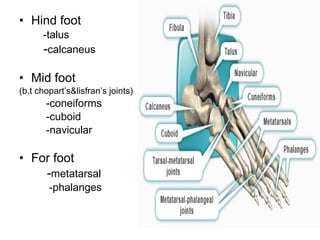
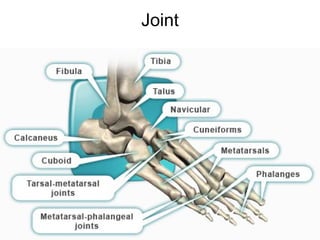
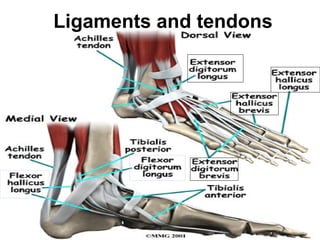
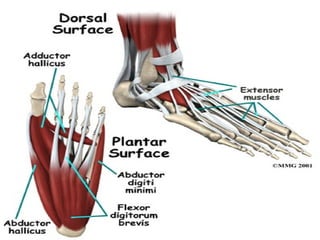
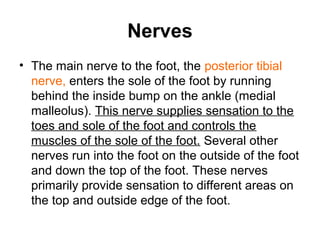
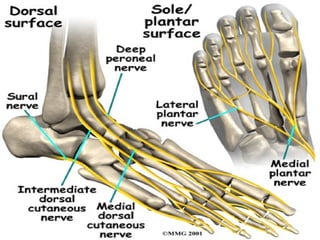
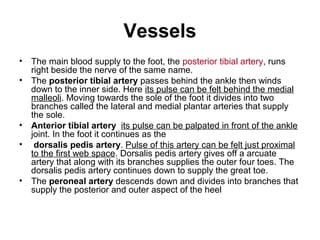
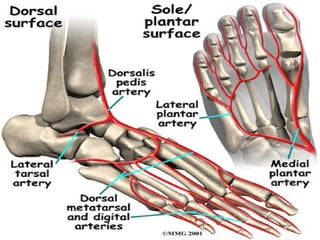
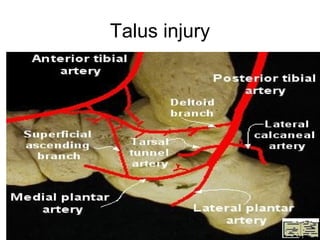
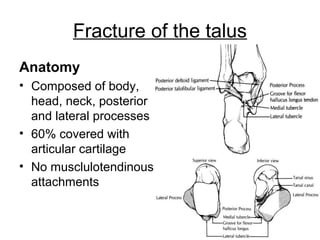
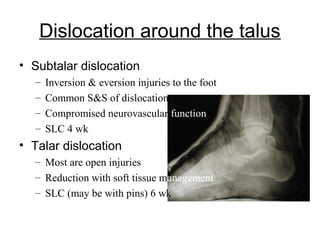
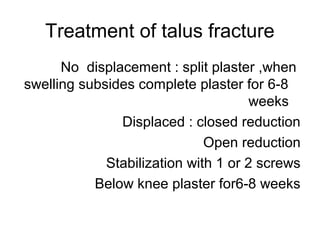
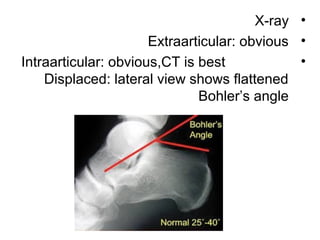
This document discusses the anatomy of the foot and injuries to the hindfoot and talus bone. It describes the bones and joints of the foot, including the tarsal bones, metatarsals, and phalanges. It also outlines the ligaments, tendons, nerves and blood vessels of the foot. Regarding injuries, it describes fractures and dislocations of the talus bone that can result from direct or indirect trauma. It notes the mechanisms of talus injuries and treatments such as closed or open reduction and internal fixation. The document also discusses calcaneal fractures, noting treatments for displaced or undisplaced fractures involve reduction, fixation, and immobilization.