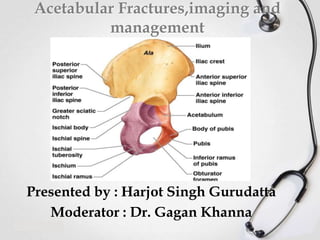
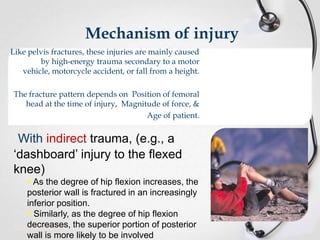
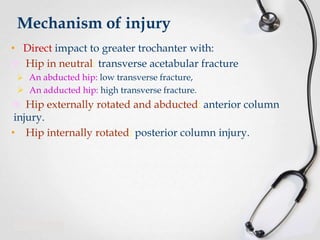
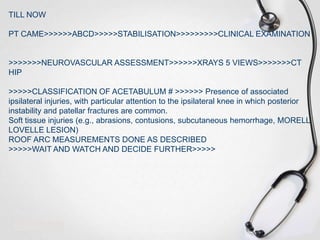
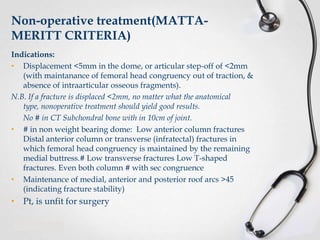
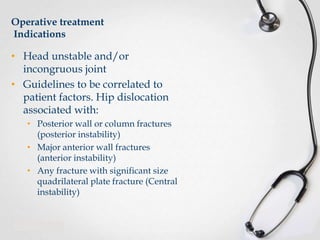
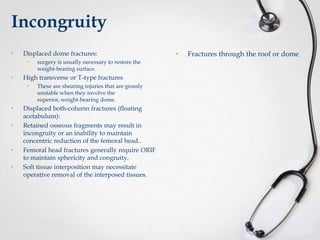
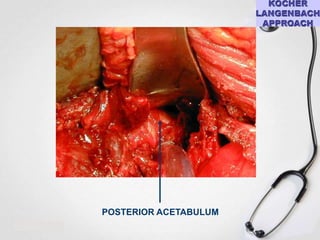
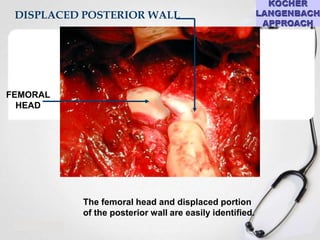
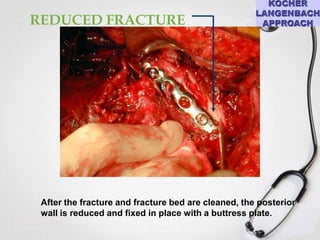
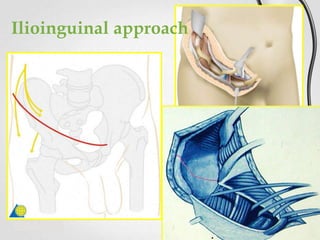
1) The document discusses acetabular fractures, including the anatomy and biomechanics of the acetabulum, classification systems, imaging, and management considerations.
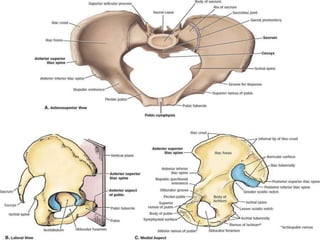
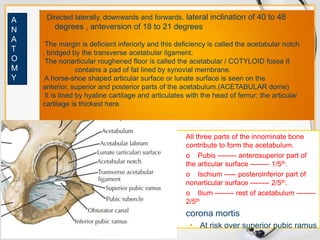
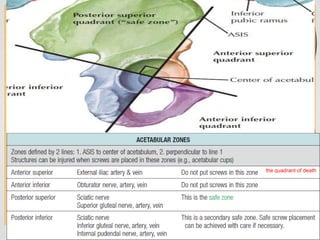
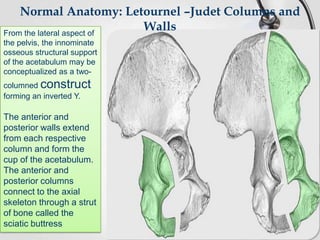
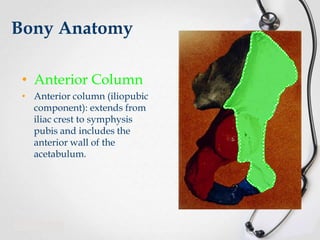
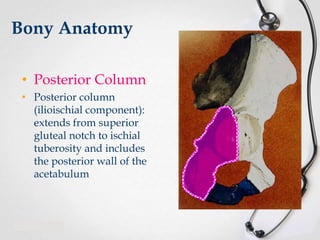
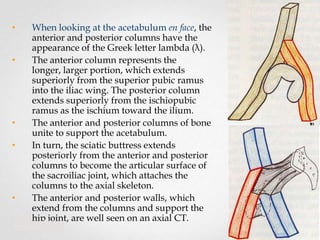
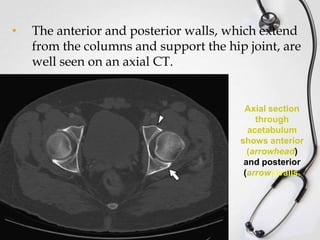
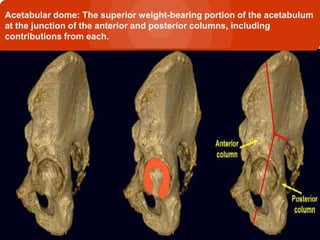
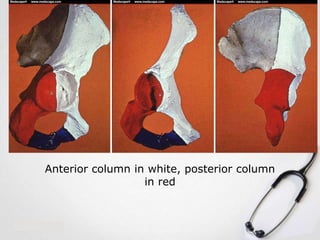
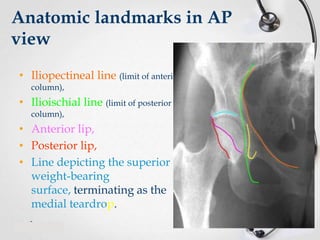
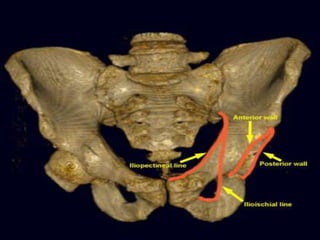
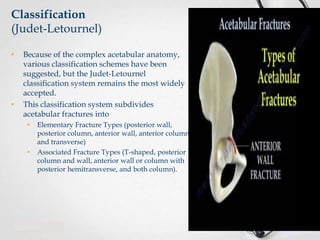
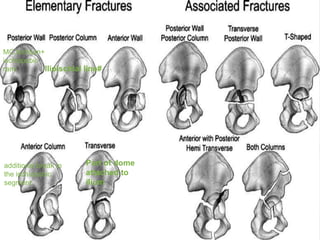
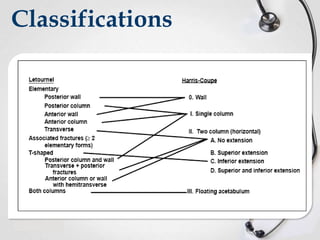
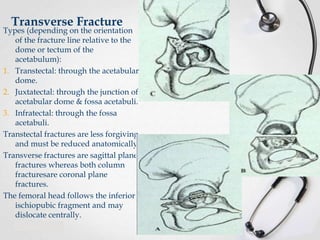
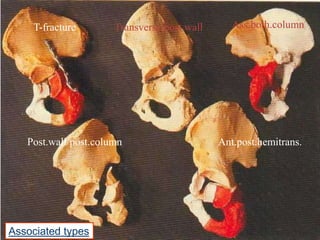
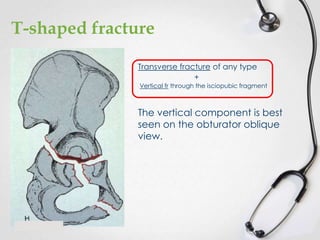
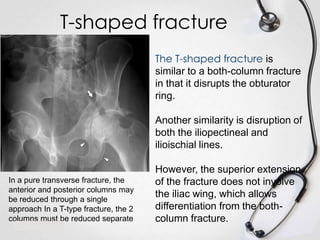
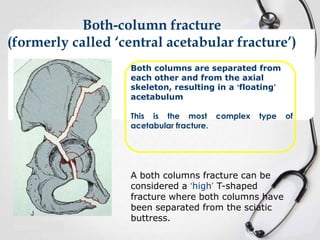
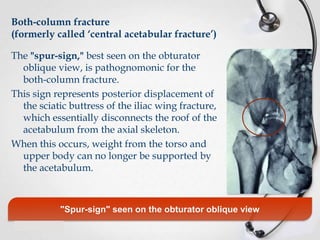
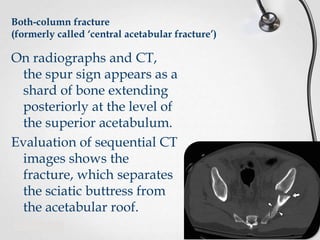
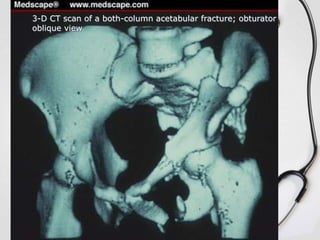
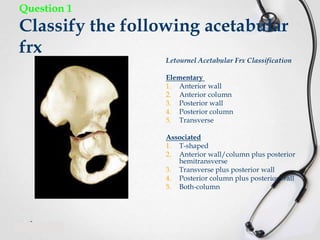
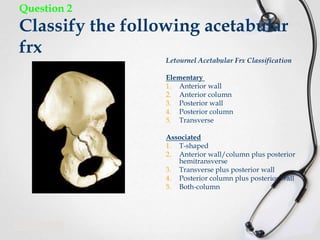
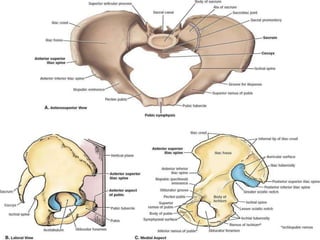
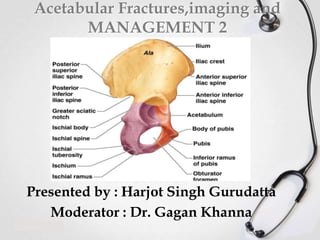
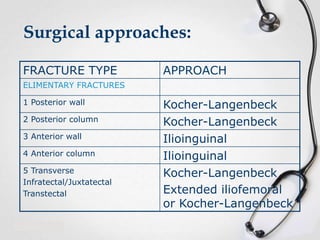
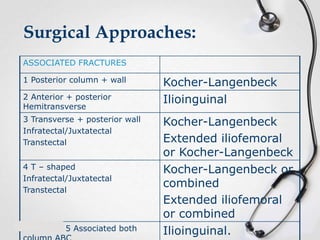
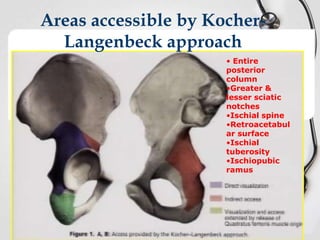
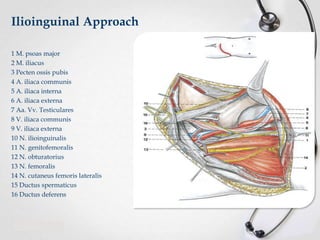
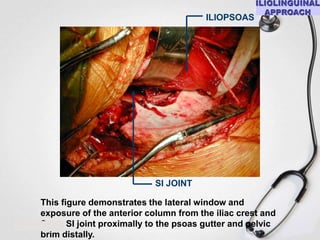
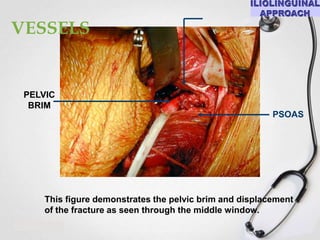
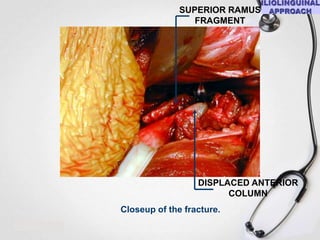
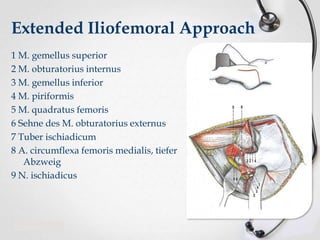
2) Key anatomical structures include the anterior and posterior columns that support the acetabulum. The Judet-Letournel classification system categorizes fractures as elementary or associated types based on involvement of the anterior column, posterior column, transverse fracture pattern, and combinations.
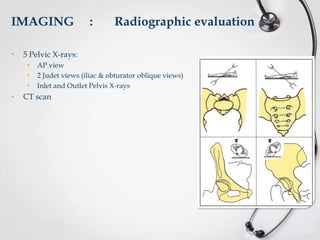
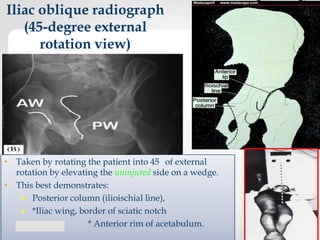
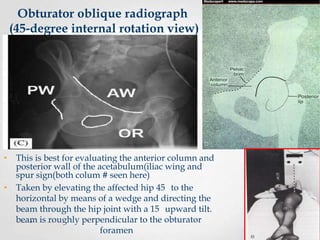
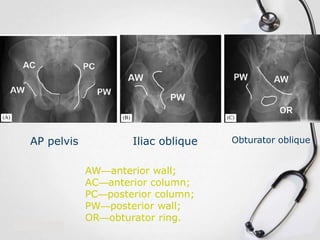
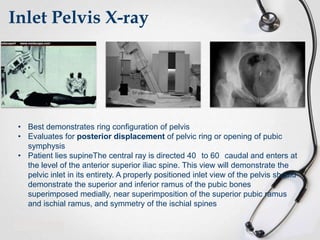
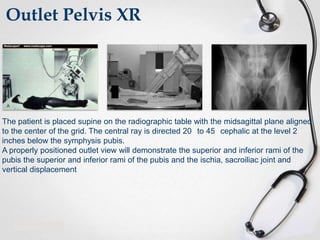
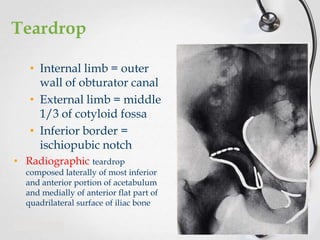
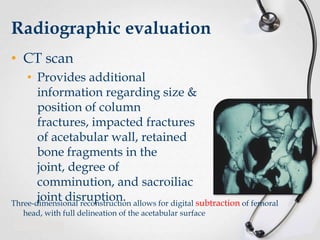
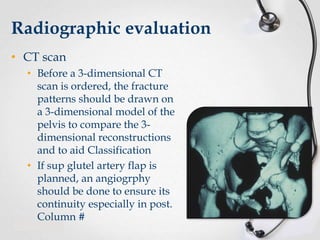
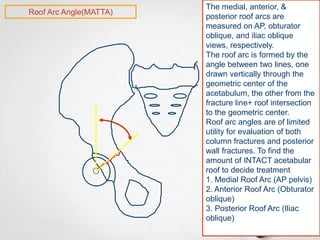
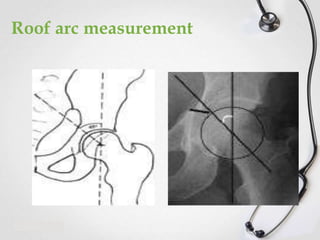
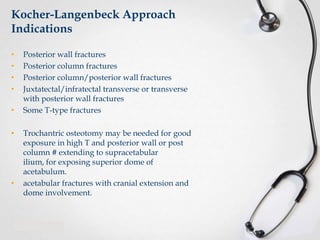
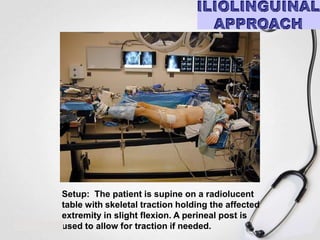
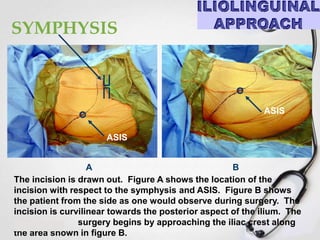
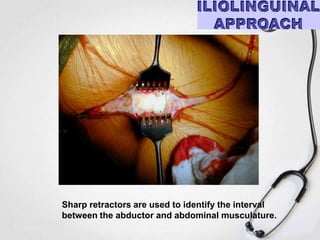
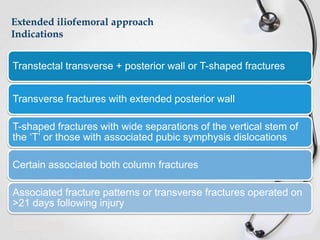
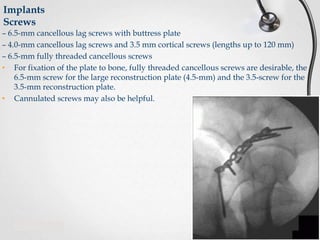
3) Evaluation involves clinical exam along with radiographs including pelvis AP, iliac and obturator oblique views, and CT scan to fully characterize the fracture pattern and guide treatment planning. Accurate classification is important for determining the proper surgical approach and management.