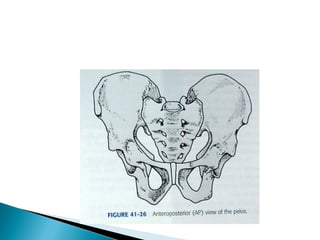
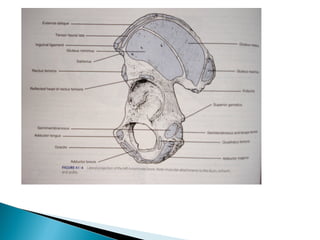
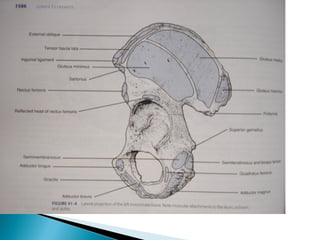
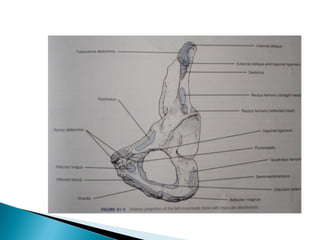
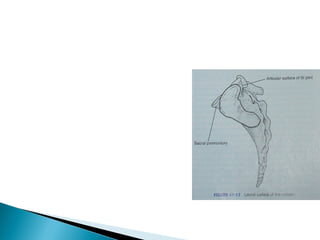
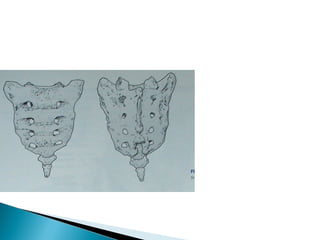
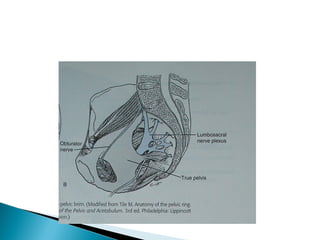
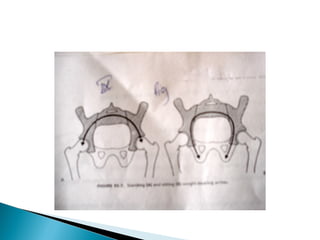
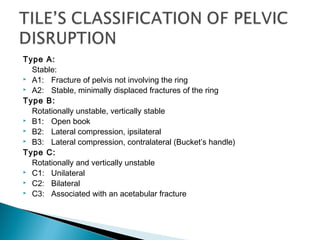
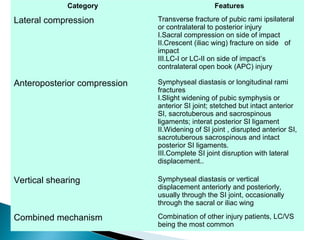
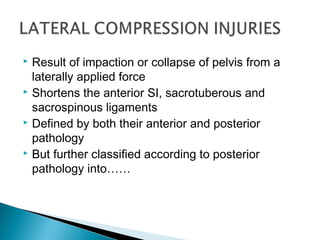
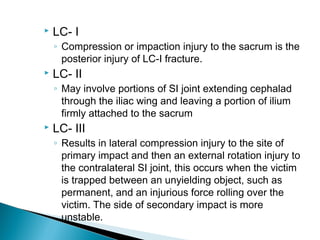
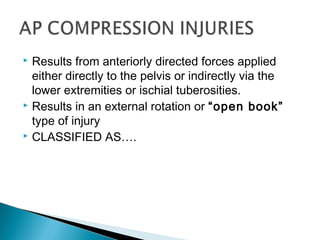
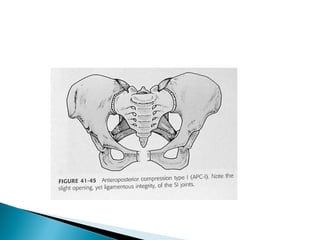
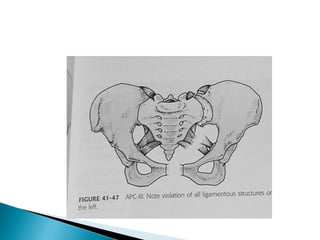
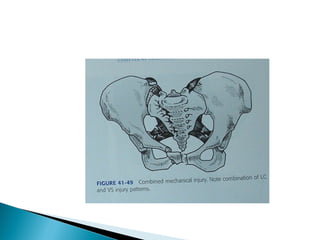
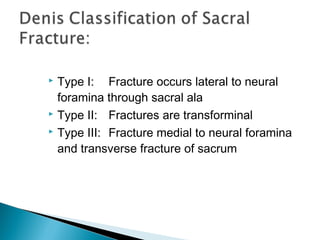
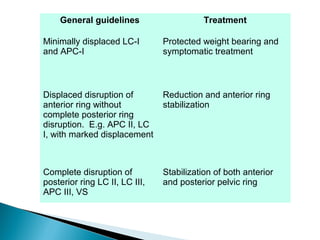
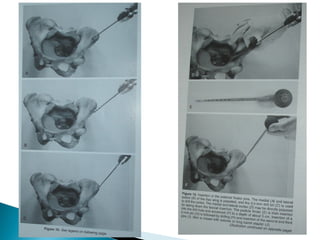
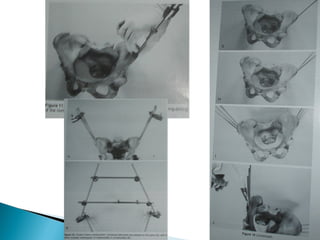
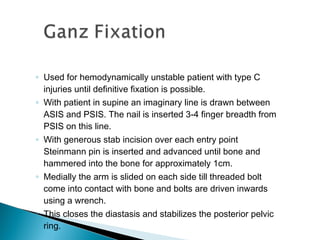
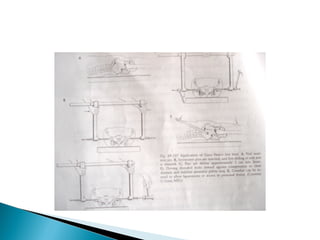
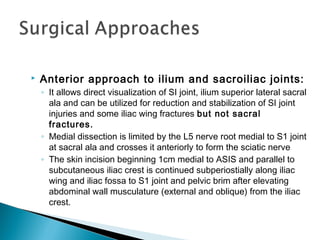
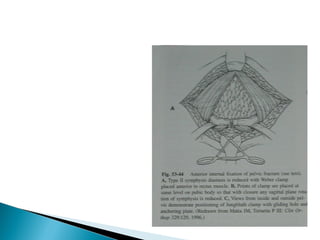
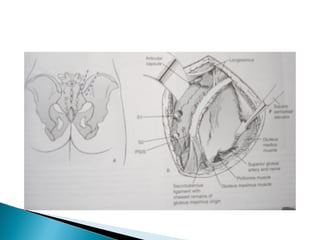
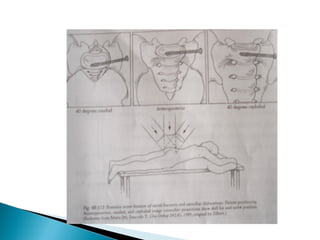
This document discusses pelvic fractures, including their anatomy, classification, mechanisms of injury, clinical evaluation, imaging, and various treatment methods. It provides an in-depth overview of pelvic ring injuries, describing different fracture patterns such as lateral compression, anteroposterior compression, and vertical shear fractures. Both non-operative and operative treatment approaches are covered, including external fixation, internal fixation of the anterior or posterior ring, and techniques for stabilizing specific fracture types.