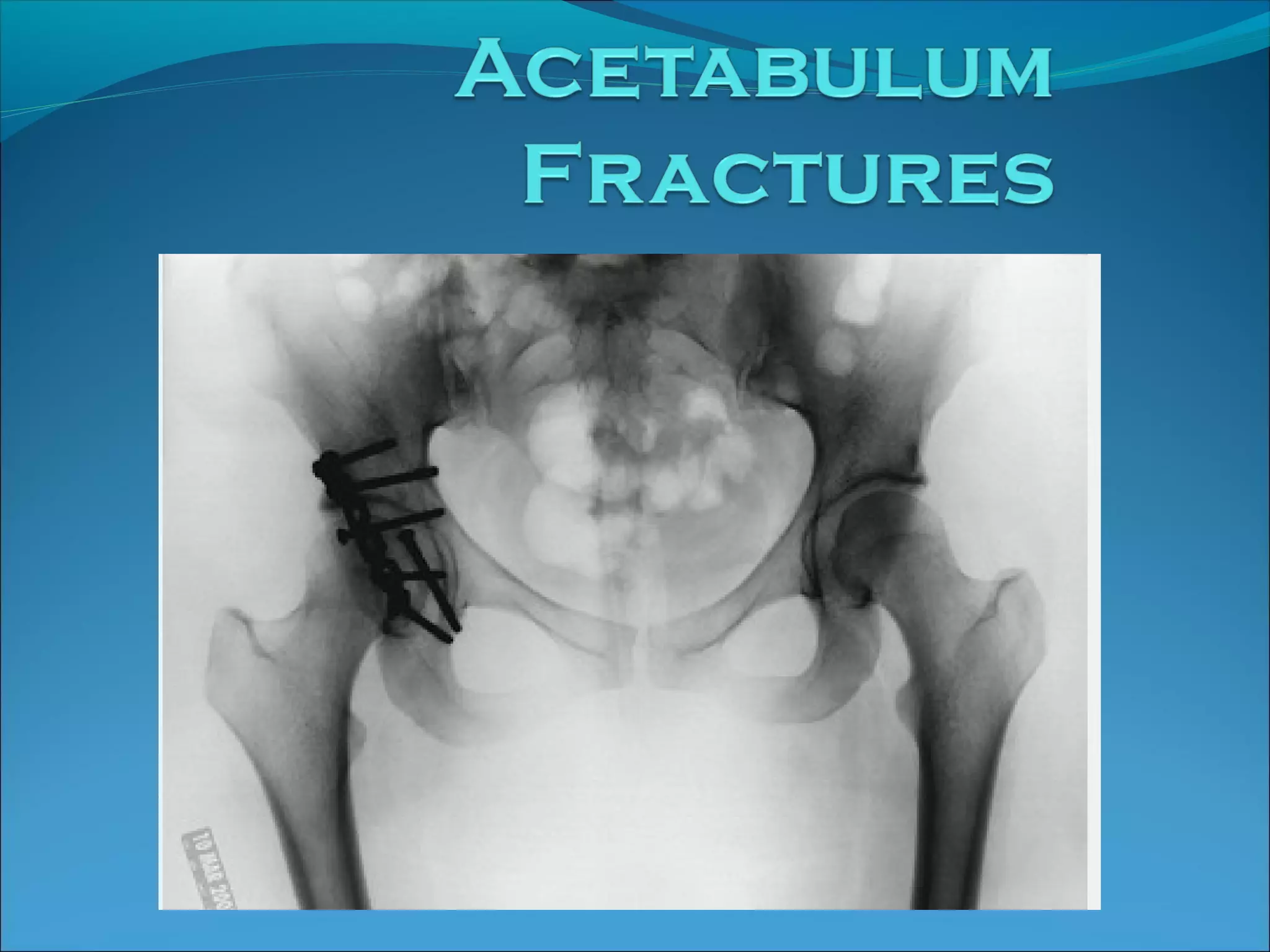
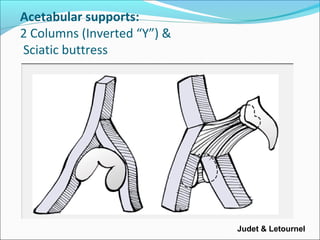
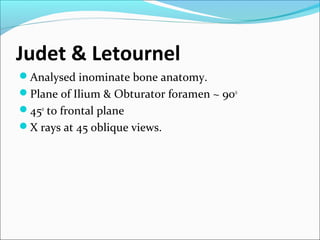
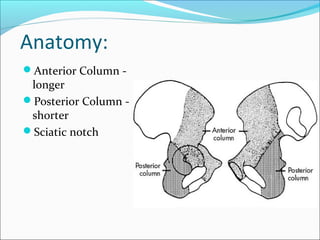
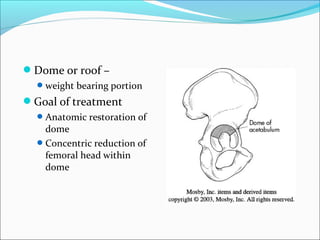
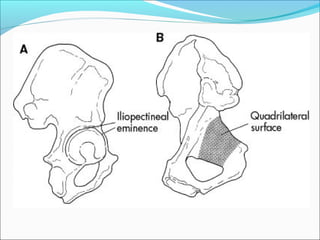
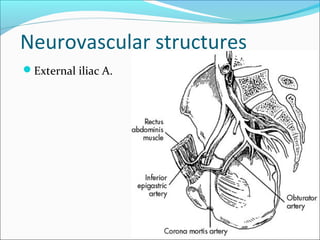
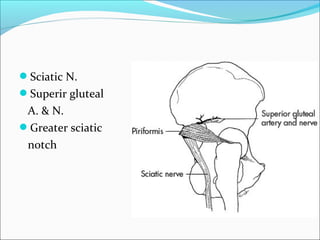
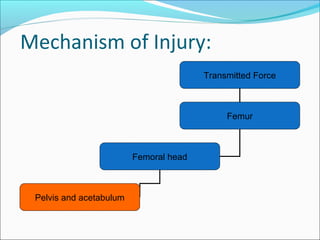
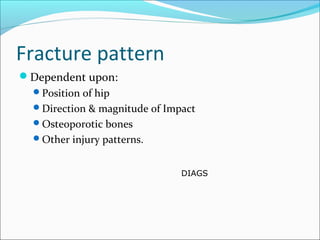
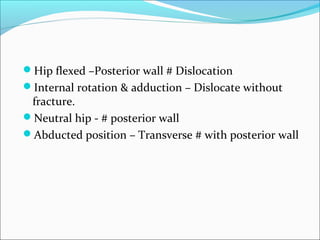
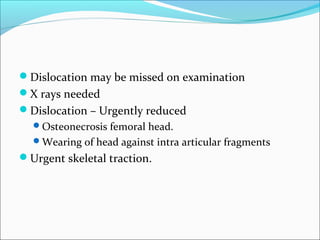
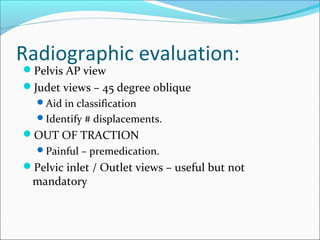
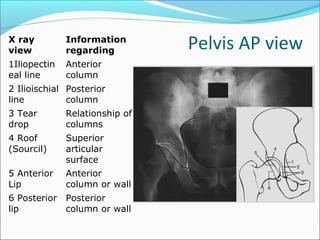
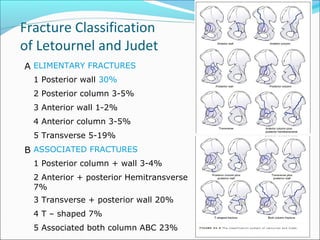
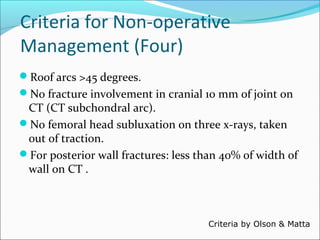
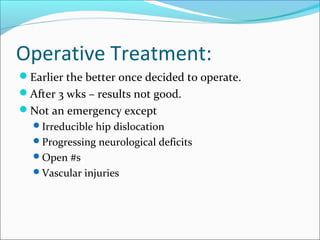
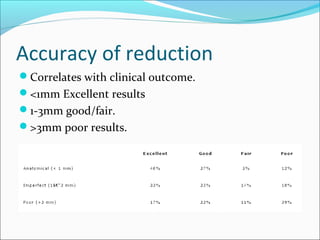
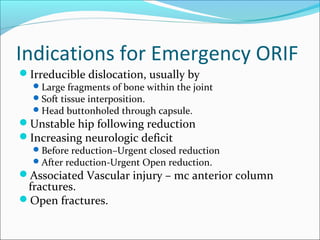
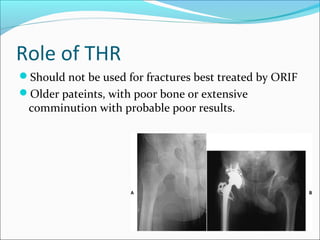
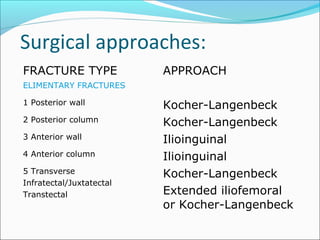
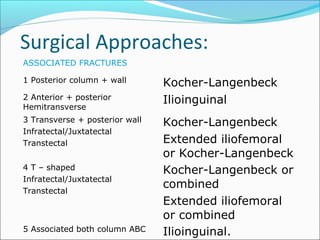
The document discusses the anatomy and classification of acetabular fractures. It notes that Judet and Letournel analyzed the anatomy of the innominate bone and established planes and angles. Acetabular fractures are classified using the Judet and Letournel or Orthopaedic Trauma Association systems. Treatment may involve non-operative management with traction or surgery depending on the fracture pattern and stability. Surgical approaches are dependent on the specific fracture location and goal is anatomic reduction to restore a congruent joint. Complications can include arthritis, heterotopic ossification, nerve injuries and infection.