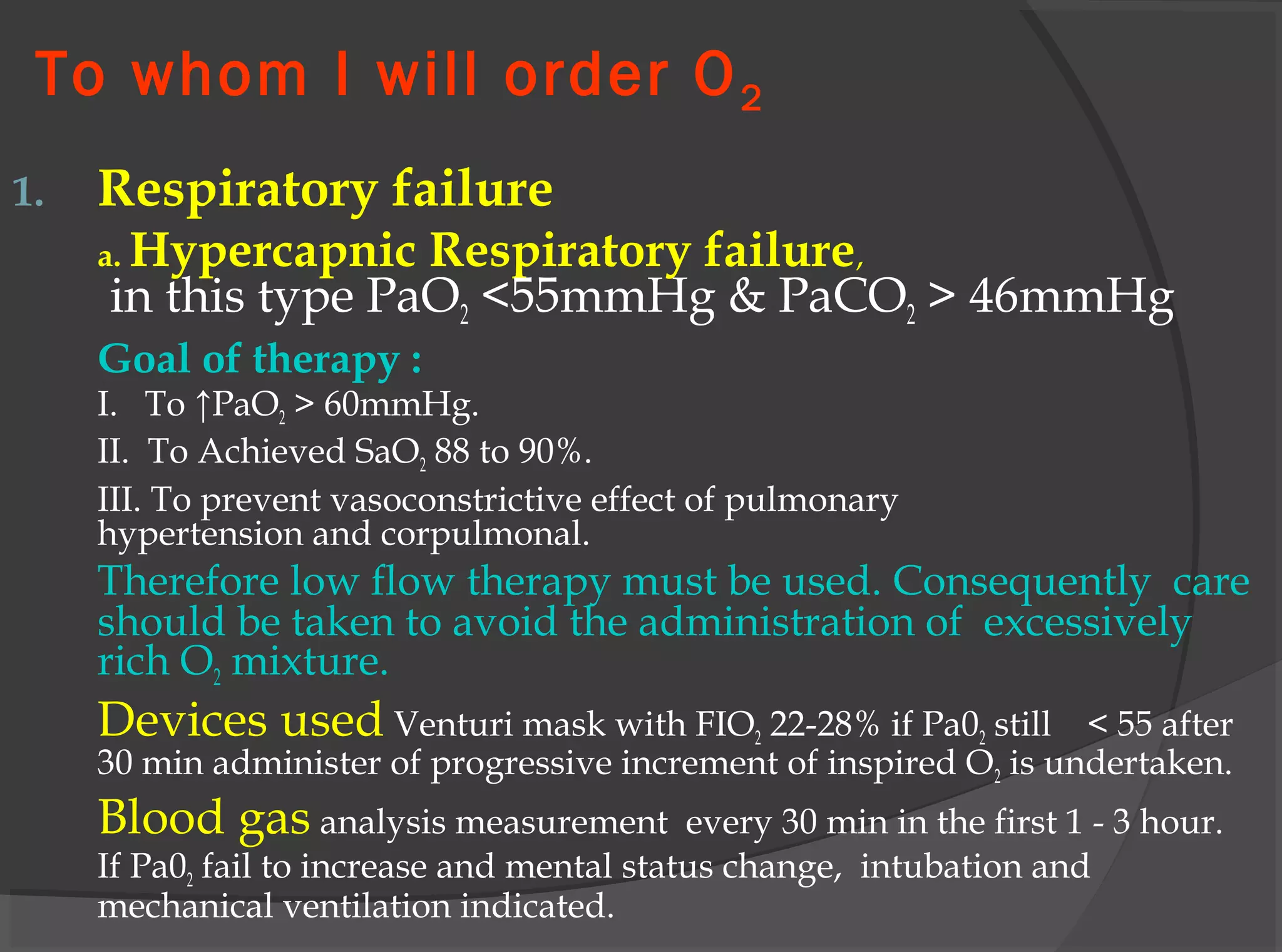
This document discusses oxygen therapy and oxygen toxicity. It aims to provide guidelines for oxygen therapy including indications, goals, delivery methods and their advantages/disadvantages. Prolonged high concentration oxygen can cause pulmonary toxicity similar to ARDS. The optimal oxygen concentration is the lowest that maintains tissue oxygenation below 60% FIO2 to avoid toxicity. Measures like mechanical ventilation and antioxidants can help prevent toxicity from prolonged high concentration oxygen.