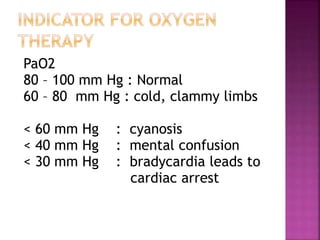
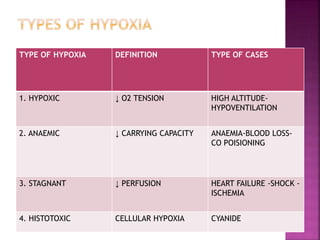
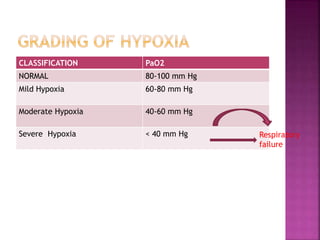
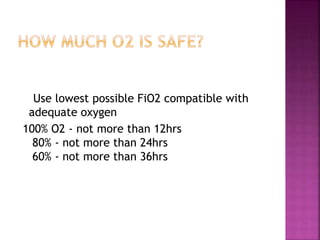
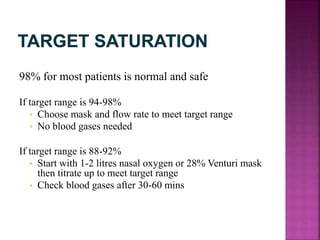
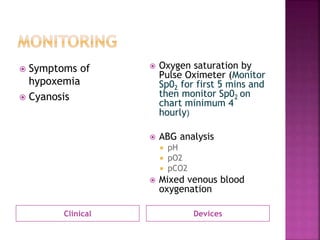
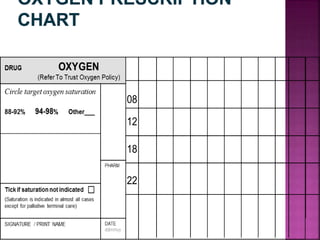
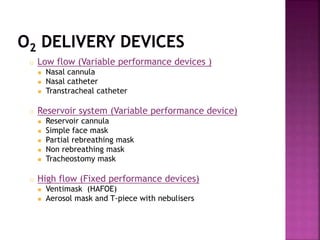
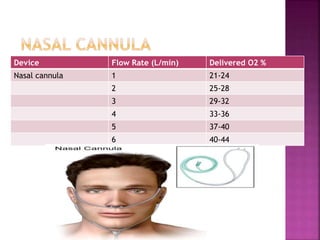
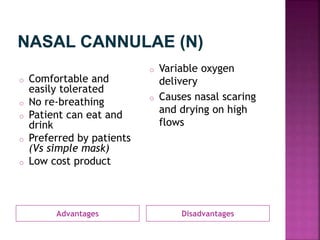
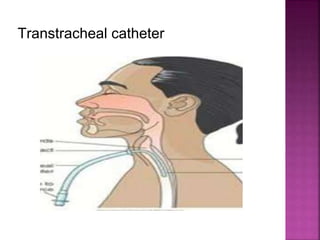
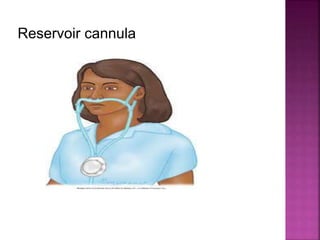
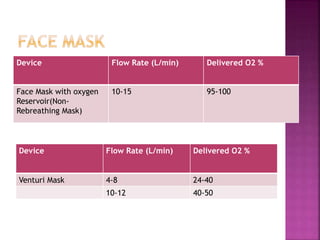
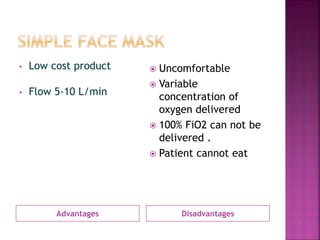
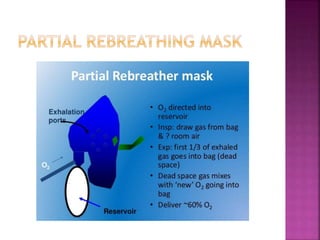
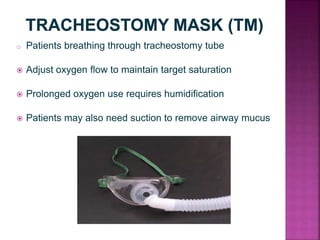
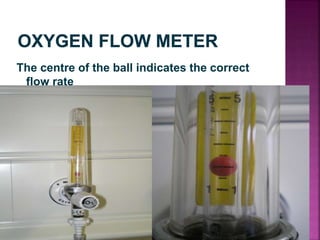
This document discusses oxygen therapy and hypoxia. It defines oxygen therapy as the administration of oxygen at concentrations greater than ambient air to treat or prevent symptoms of hypoxia. It then discusses types of hypoxia based on low oxygen tension, anemia, poor perfusion, and cellular hypoxia. Clinical signs of hypoxia like cyanosis and oxygen saturation levels are also summarized. The document provides guidance on oxygen devices, flow rates, concentrations delivered, advantages and disadvantages of different devices like nasal cannulas, masks, and indications for long term oxygen therapy.