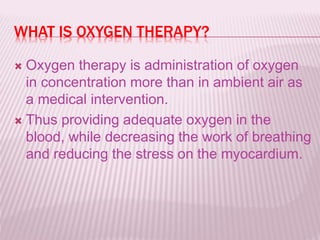
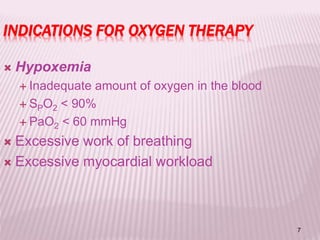
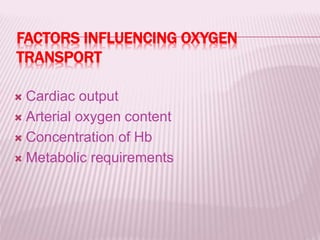
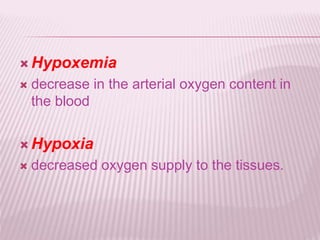
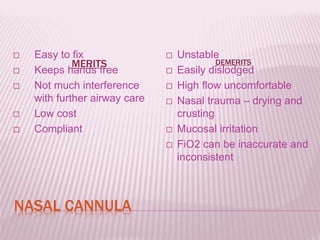
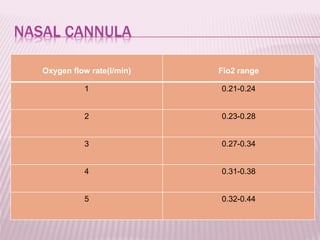
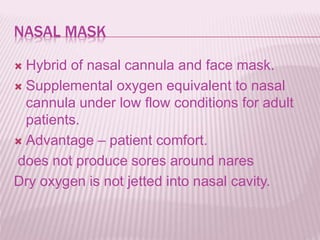
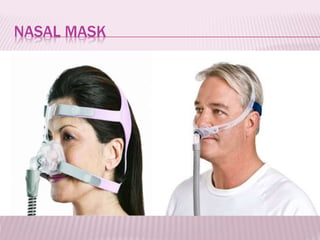
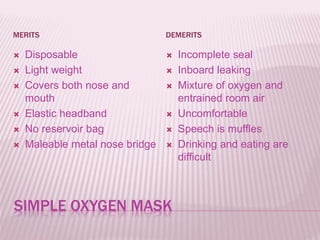
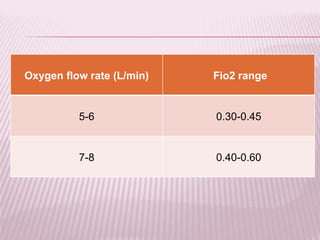
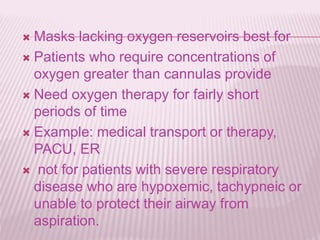
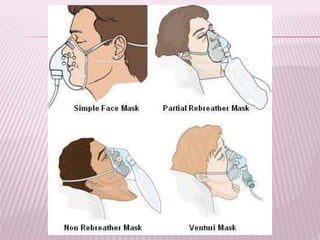
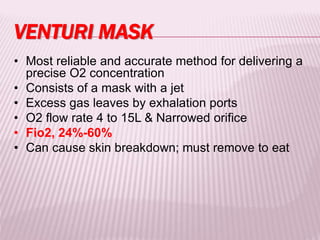
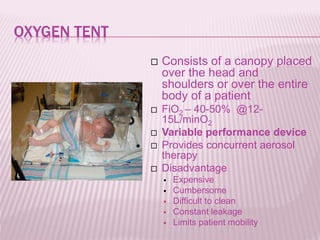
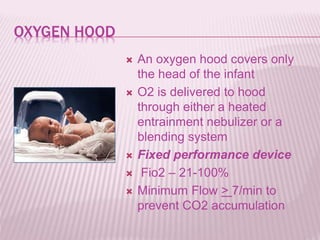
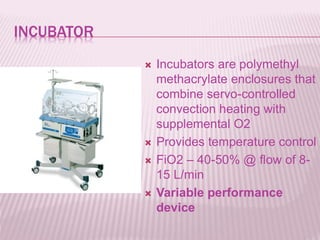
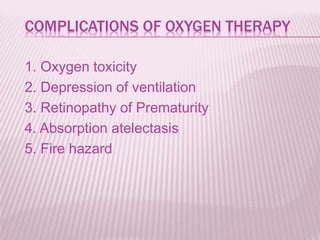
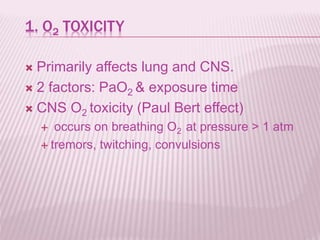
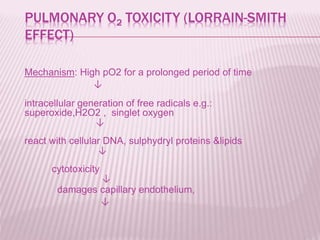
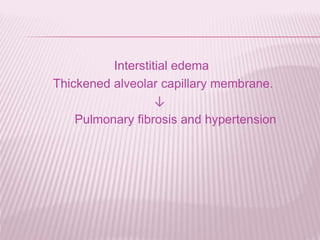
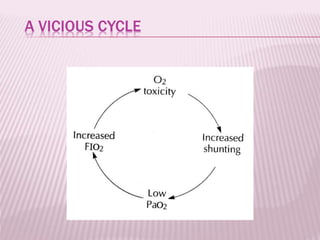
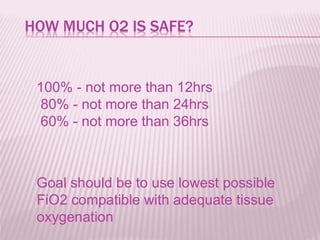
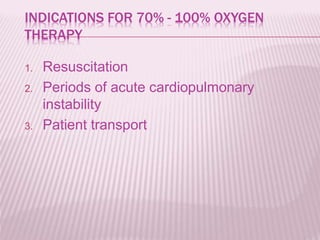
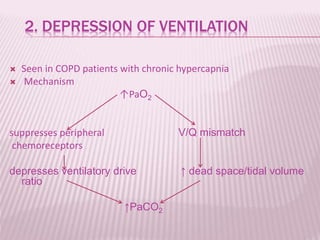
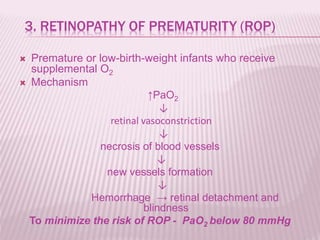
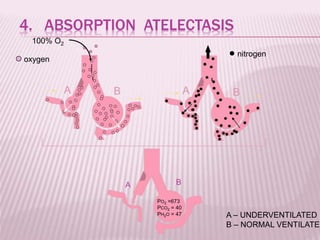
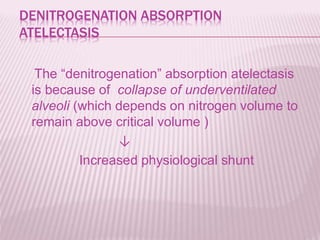
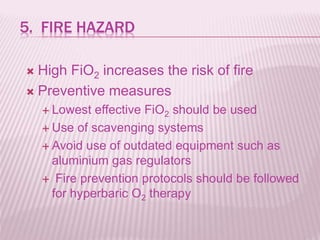
Oxygen therapy involves administering supplemental oxygen to increase oxygen levels in the blood. It is used when a patient has hypoxemia or low blood oxygen levels. Different devices are used to deliver oxygen depending on the patient's condition and oxygen needs. The main devices discussed are nasal cannulas, masks, venturi masks, and high flow devices. Potential complications of oxygen therapy include oxygen toxicity if delivered at too high of concentrations for too long, depression of ventilation, retinopathy of prematurity in infants, and fire hazards. Care must be taken to closely monitor patients on oxygen therapy.