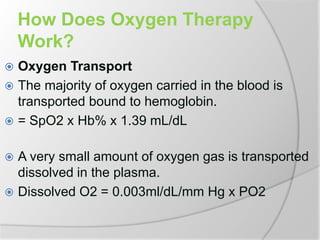
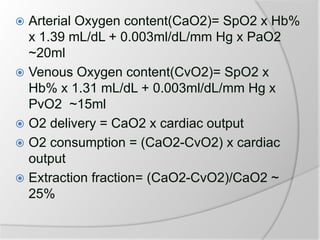
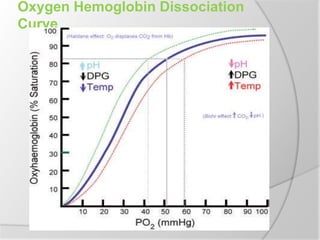
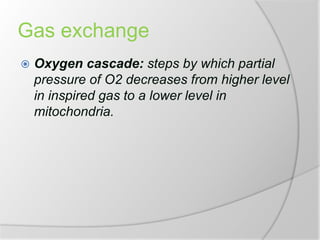
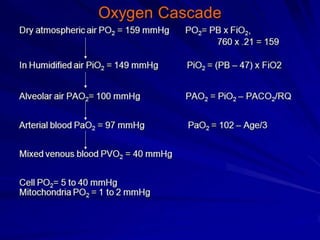
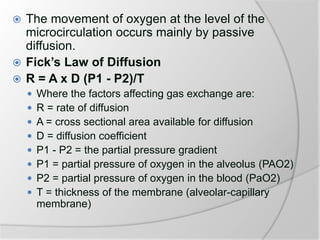
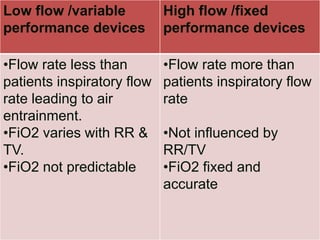
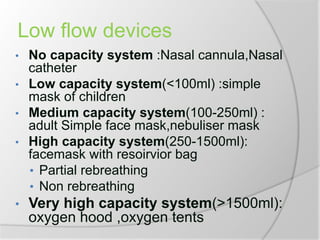
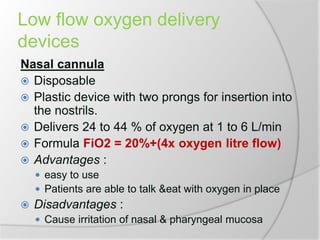
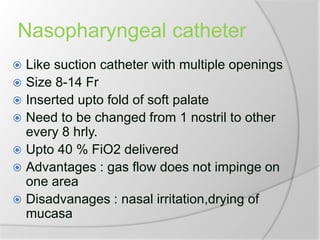
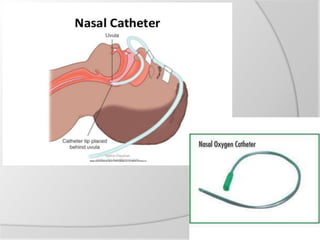
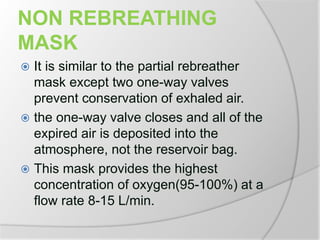
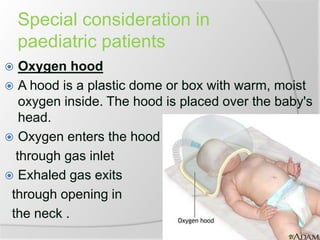
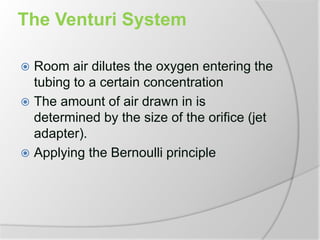
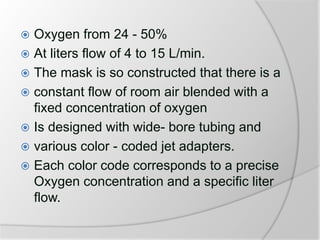
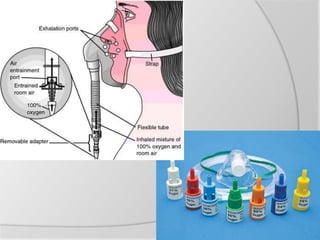
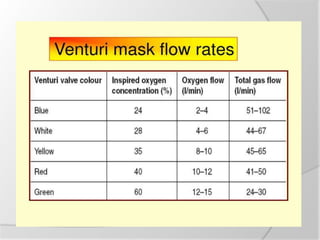
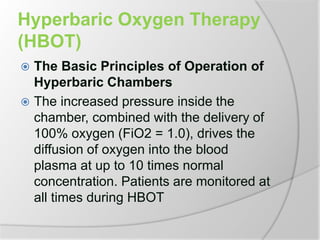
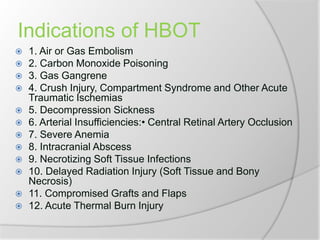
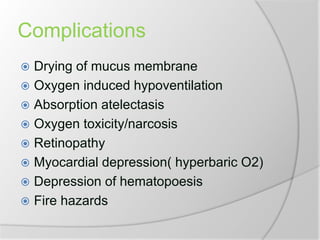
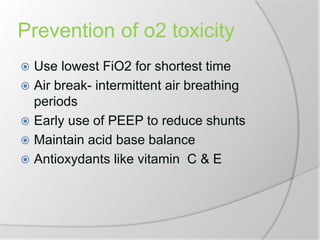
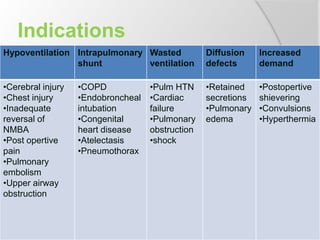
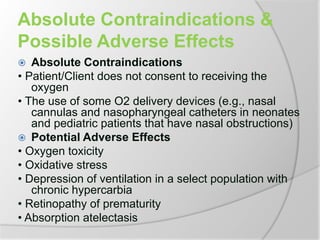
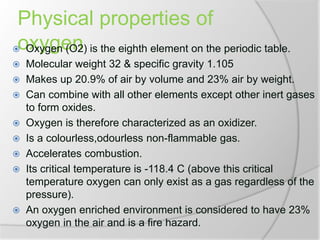
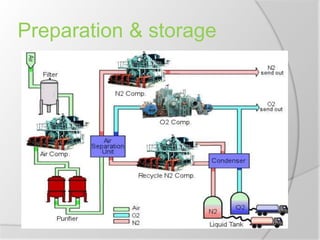
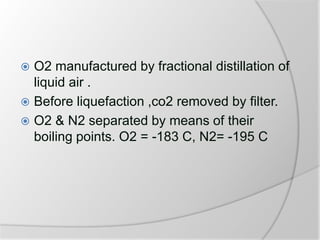
The document outlines the principles and practices of oxygen therapy, including its definitions, goals, indications, contraindications, delivery systems, and potential adverse effects. It details various oxygen delivery devices, their mechanisms, and calculations for use in clinical settings, along with the physiological aspects of oxygen transport and gas exchange. The document also highlights special considerations for pediatrics, high-flow systems, and complications related to oxygen therapy.
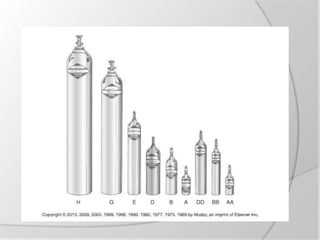
![Calculation of duration of
flow
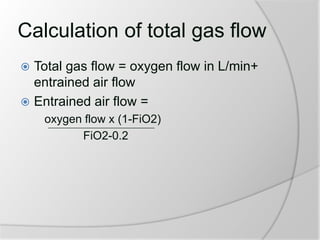
To calculate how long a cylinder will last based
on the size of the cylinder and continuous flow
rate, the following formula can be used:
Duration of Flow in minutes =
[current gauge pressure in psi x cylinder
factor]/ Flow rate in liters per minute
Some examples of cylinder factors for different
sized cylinders are:
D cylinder 0.16
E cylinder 0.28
M cylinder 1.56](https://image.slidesharecdn.com/oxygentherapy-180627125931/85/Oxygen-therapy-13-320.jpg)