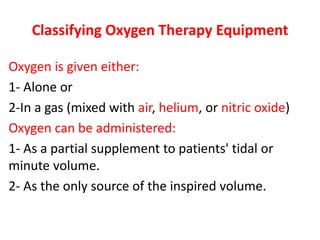
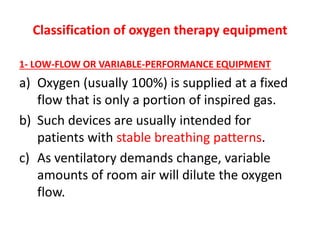
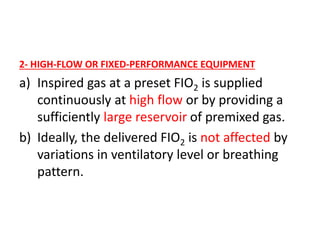
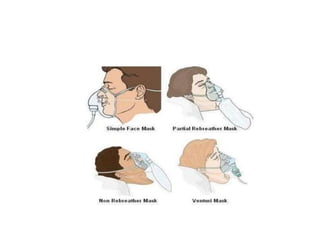
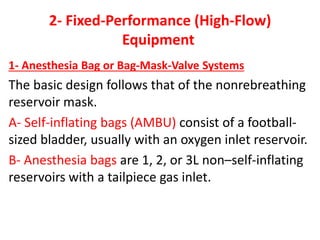
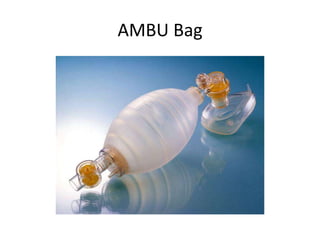
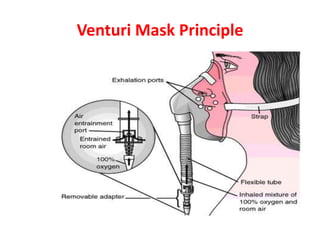
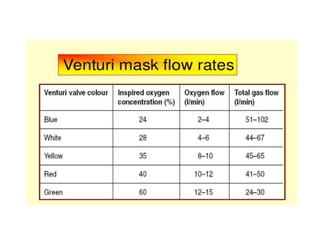
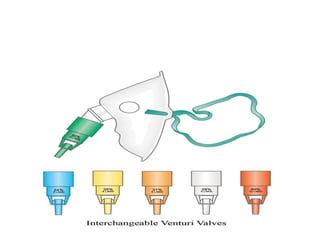
1) Oxygen therapy equipment can be classified as either low-flow/variable-performance equipment or high-flow/fixed-performance equipment. Low-flow equipment includes nasal cannulas and masks, while high-flow includes anesthesia bags and venturi masks.
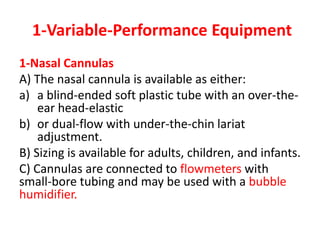
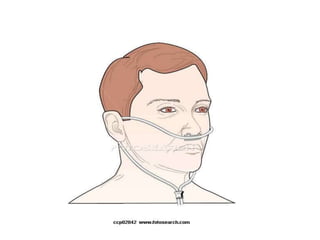
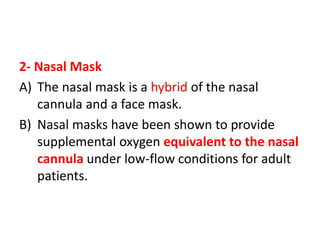
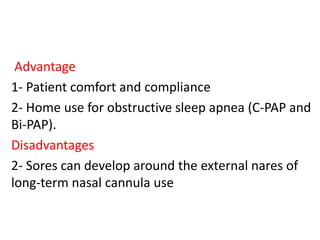
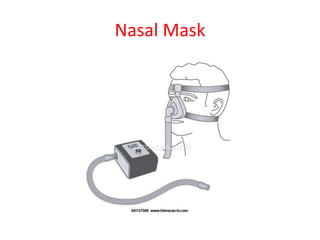
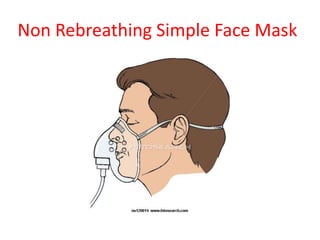
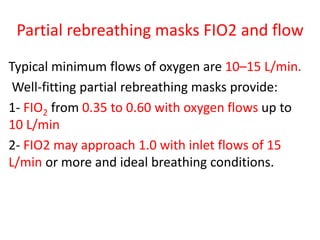
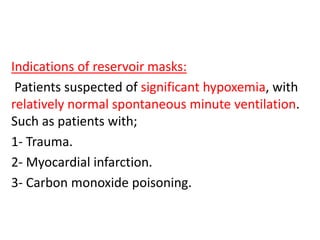
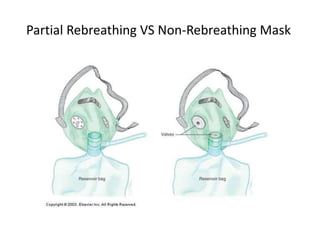
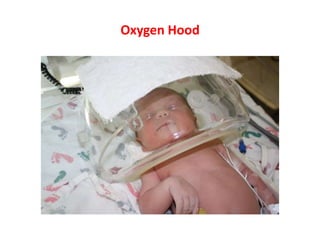
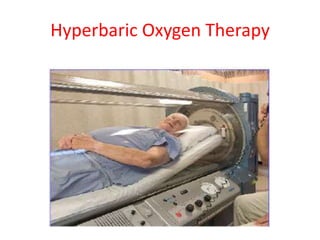
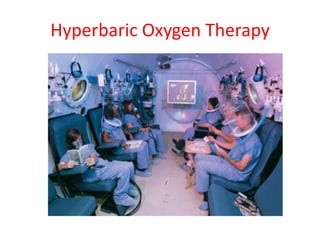
2) Key oxygen therapy devices include nasal cannulas, nasal masks, simple face masks, reservoir masks, venturi masks, nebulizers, oxygen hoods, and hyperbaric oxygen chambers. Each device has advantages and disadvantages for delivering different concentrations of oxygen under varying conditions.
3) Proper use and settings of oxygen therapy equipment, including sufficient gas flow, addressing leaks, and patient fit are important to ensure patients receive the targeted concentration of oxygen