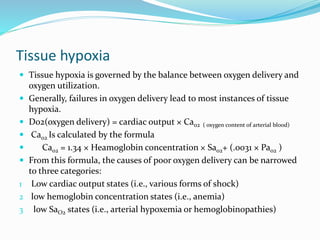
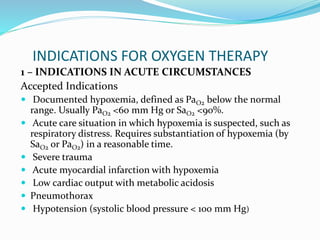
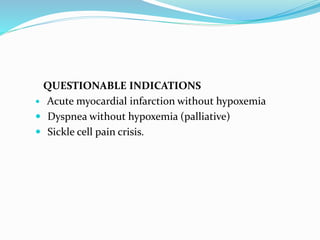
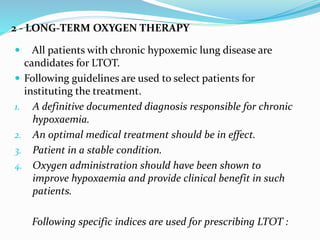
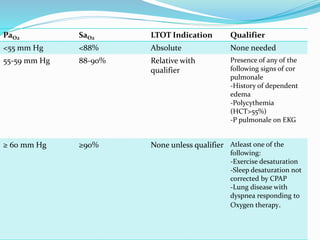
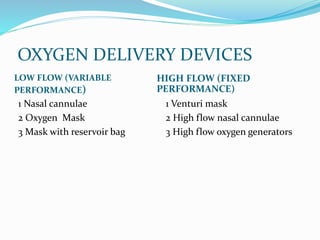
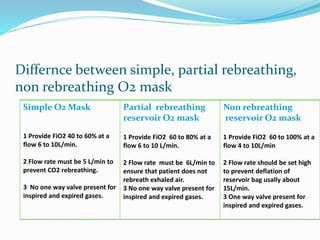
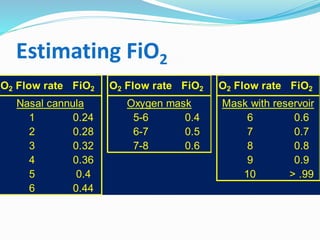
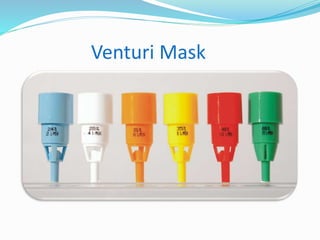
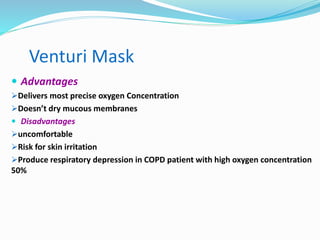
Oxygen therapy involves prescribing supplemental oxygen to ensure adequate oxygen delivery to tissues. It is considered a medical treatment and requires a doctor's order specifying the oxygen concentration, flow rate, and duration. Oxygen therapy is used to treat hypoxemia in both acute and chronic conditions. Different devices are used to deliver oxygen at either low or high concentrations, with masks being variable performance devices and venturi masks or high flow cannulas providing fixed performance. Proper use and settings are important for safety and effectiveness.