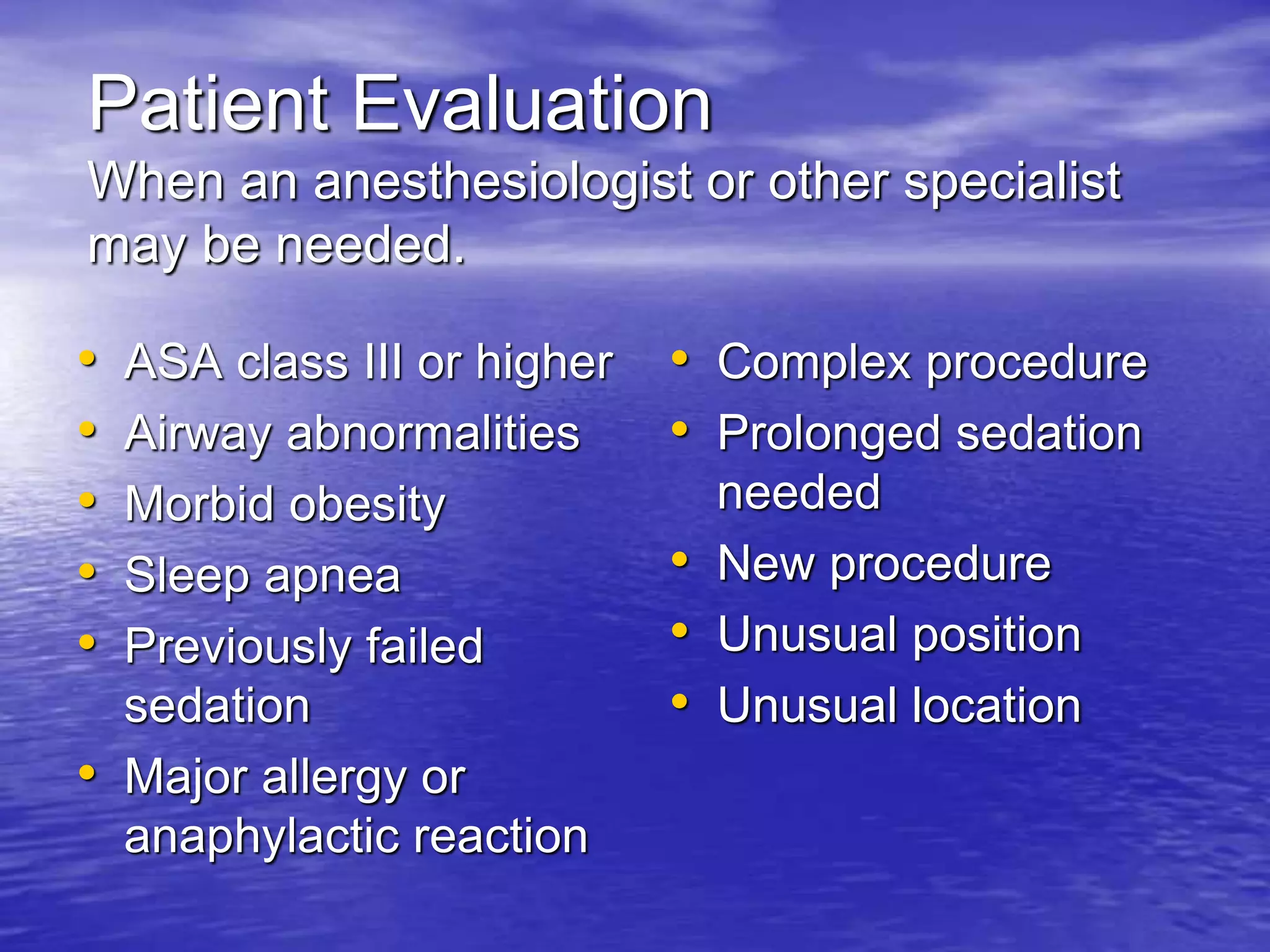
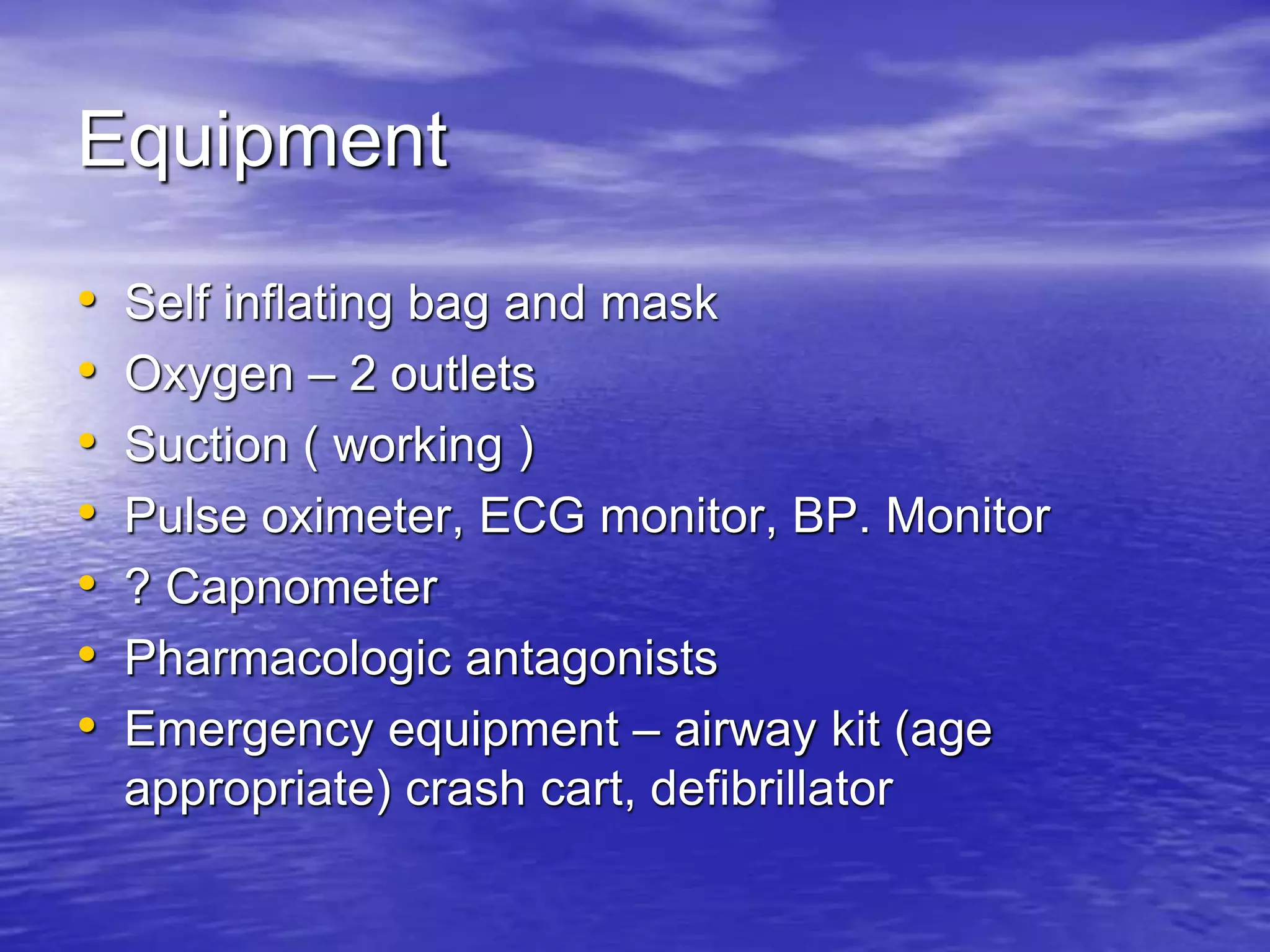
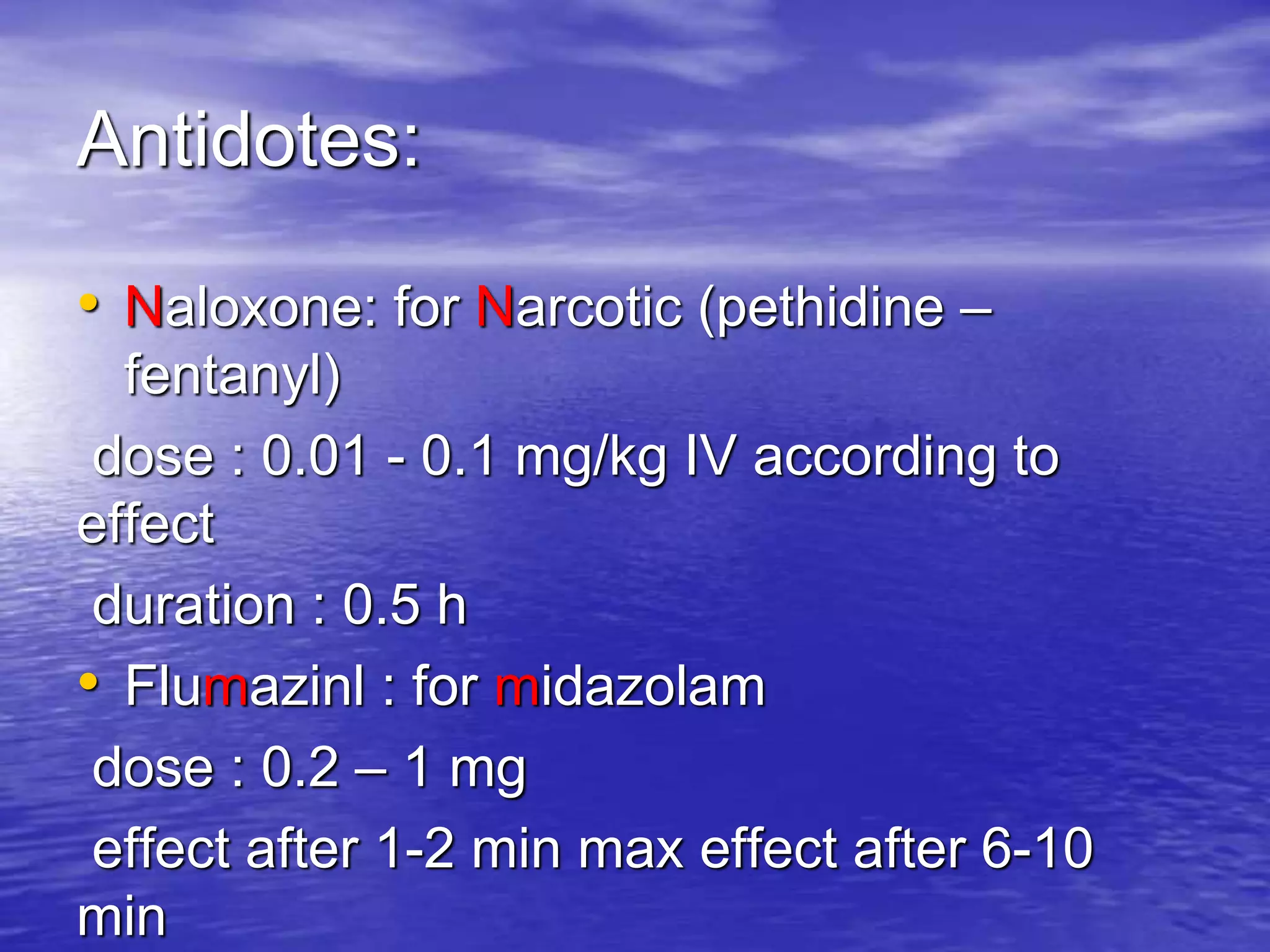
This document provides guidelines for moderate sedation/analgesia (conscious sedation). It defines levels of sedation from minimal to general anesthesia. Moderate sedation involves patients responding purposefully to verbal commands with spontaneous breathing. The guidelines discuss patient evaluation, monitoring, personnel, equipment, drugs and discharge criteria for providing moderate sedation. Proper patient screening, credentialed practitioners and personnel, appropriate facilities and emergency equipment are emphasized to minimize risks while allowing benefits of sedation for certain medical procedures.