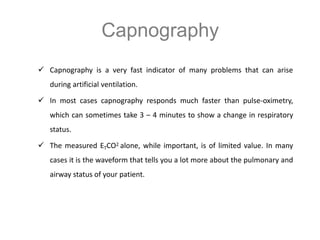
1) Capnography refers to the measurement of carbon dioxide in exhaled gas and can be used to monitor ventilation status.
2) It was first introduced in 1943 but the early devices were large and impractical.
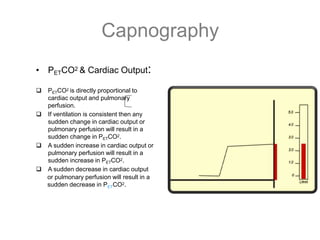
3) Capnography is now widely used in healthcare to monitor patients during procedures like intubation, sedation, mechanical ventilation and general anesthesia by providing information on respiratory and perfusion status.