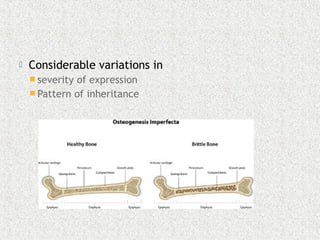
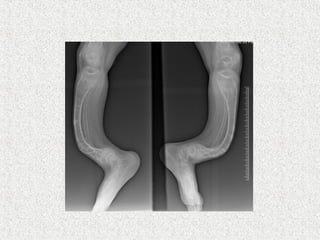
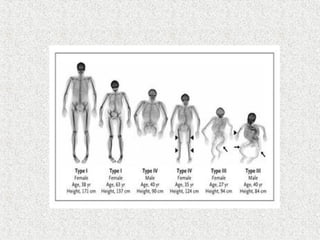
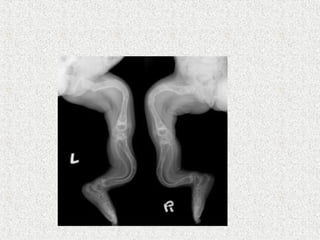
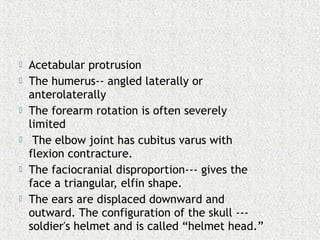
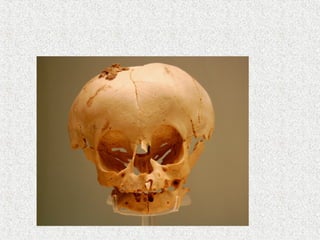
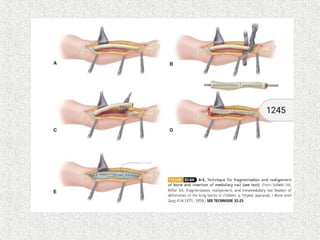
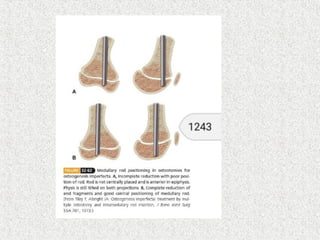
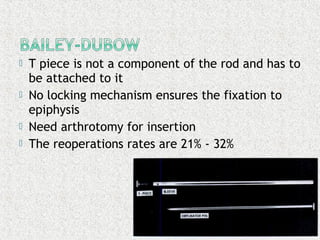
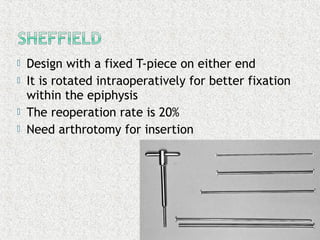
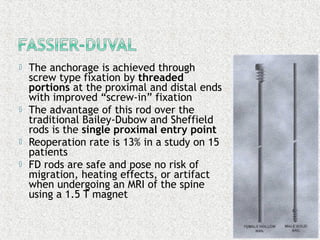
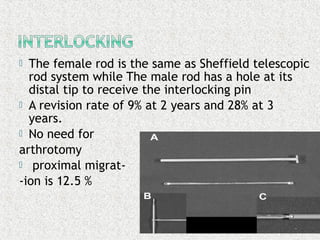
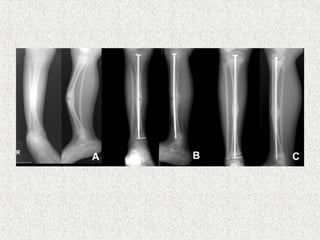
This document discusses osteogenesis imperfecta (OI), also known as brittle bone disease. It is a genetic disorder characterized by fragile bones that fracture easily, as well as other connective tissue problems. The document covers the classification, clinical features, inheritance patterns, radiographic findings, complications, and treatment options of OI, including various intramedullary rodding systems used to treat long bone deformities.