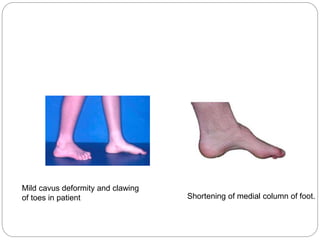
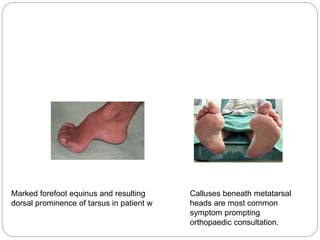
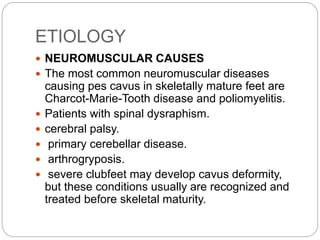
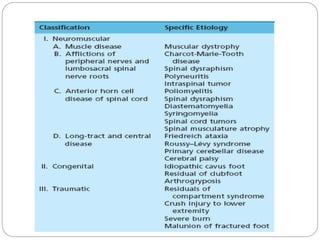
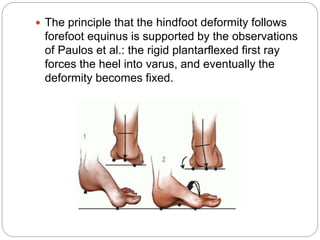
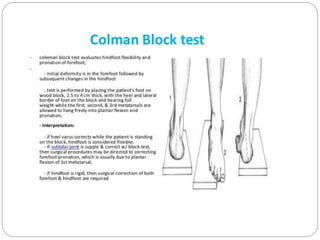
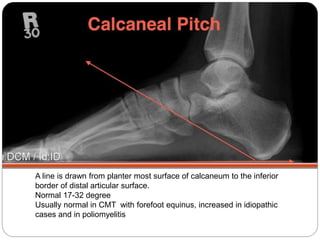
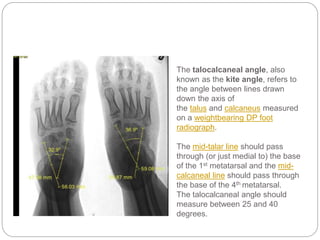
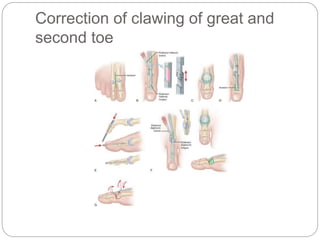
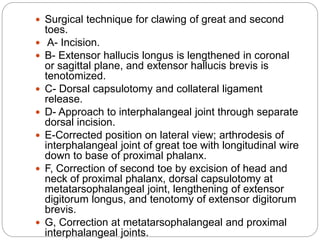
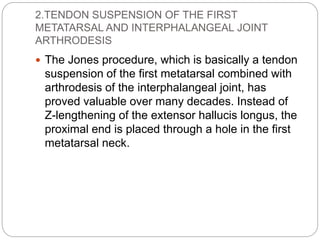
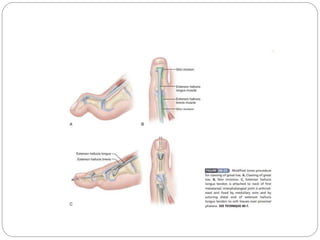
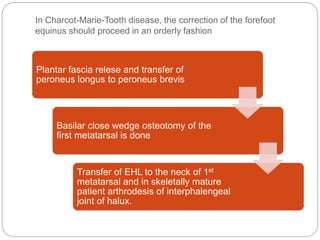
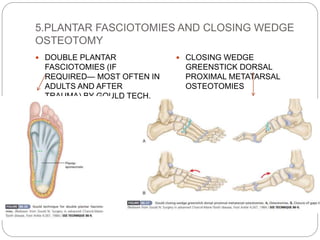
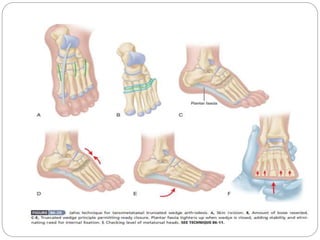
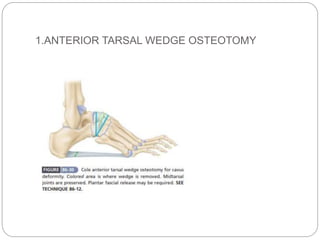
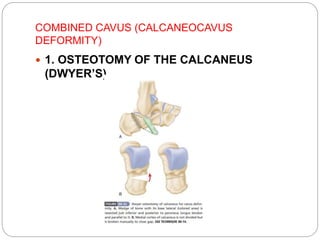
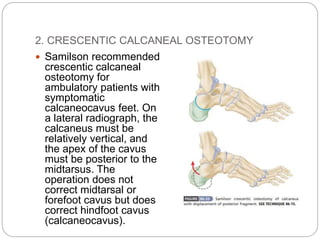
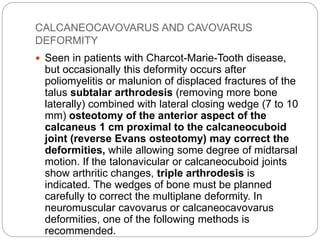
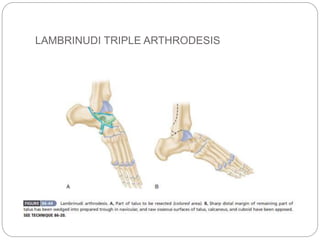
This document defines and describes cavus foot, including its causes, clinical features, diagnosis, and treatment options. A cavus foot has an abnormally high arch and accompanying toe deformities. Causes include neuromuscular conditions like Charcot-Marie-Tooth disease and polio. Clinical features include a high arch and clawing of the toes. Diagnosis involves physical exam and x-rays. Treatment depends on flexibility and severity but may include tendon lengthening, osteotomies, and joint fusions to correct deformities in the forefoot, midfoot, and hindfoot. The goal is to create a plantigrade foot.