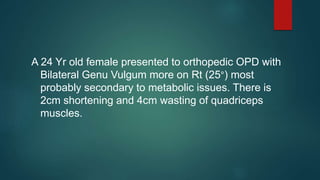
A 24-year-old female presented with bilateral genu vulgum (knock knees), more pronounced on the right side at 25 degrees, likely due to a metabolic issue. Genu vulgum is an abnormal angular deformity of the lower limbs where the legs are shifted outward from the midline. Treatment depends on the patient's age, magnitude of deformity, location of deformity, and underlying cause. For younger patients or less severe cases, conservative treatment may be sufficient, while older patients or more severe cases may require corrective osteotomy surgery.



![Evaluation of Patient : Exam
Height & weight
Percentile for age
Shortening of extremity relative to trunk
Appearance of lower limb during standing and gait
Location of deformity
Distance between medial femoral condyle [less than 6 cm]
Distance between medial maleolus [less than 8 cm]](https://image.slidesharecdn.com/genu20vulgum-220720115017-0a37160a/85/Genu-Valgum-pptx-9-320.jpg)