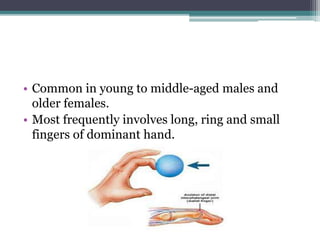
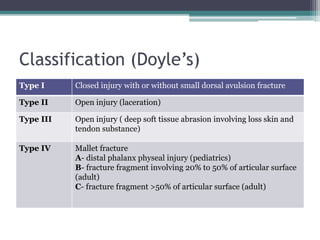
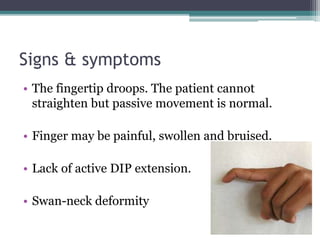
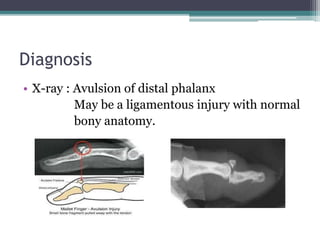
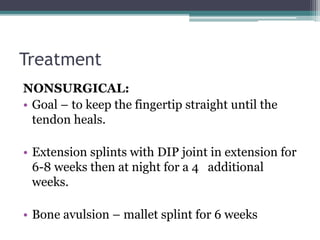
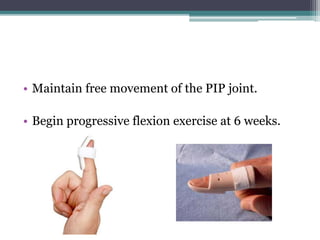
Mallet finger, or drop finger, is a deformity of the finger caused by damage to the extensor tendon below the DIP joint, preventing straightening of the fingertip. It most commonly occurs in the long, ring, or small finger of the dominant hand in young males after the fingertip is forcibly bent backwards. Treatment depends on the severity of the injury but generally involves splinting the finger to keep the DIP joint straight as the tendon heals, usually for 6-8 weeks. Surgery may be needed for open injuries, large bone fragments, or if non-surgical treatment is unsuccessful. Complications can include an extensor lag deformity or swan neck deformity if not properly