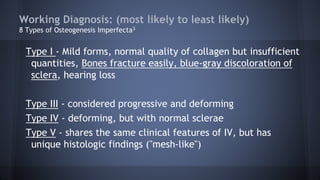
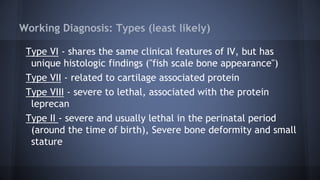
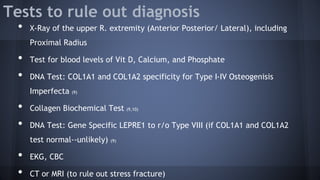
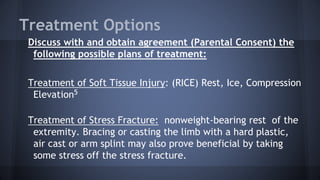
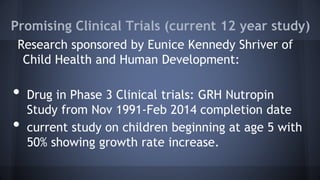
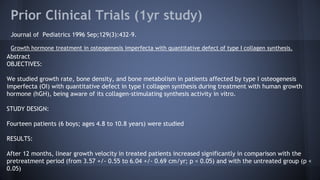
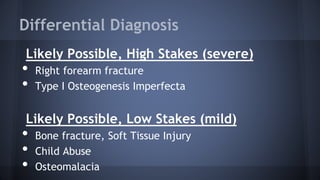
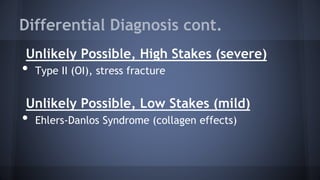
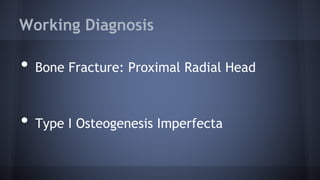
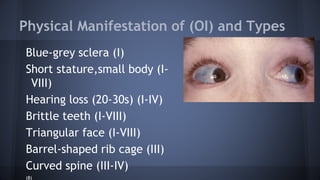
This document presents a case of a 5-year-old male brought in with excruciating right arm pain after falling off the couch. Examination revealed swelling and tenderness in the right arm with bruising in various stages on the legs and arms. The differential diagnosis included a right forearm fracture, Type I Osteogenesis Imperfecta, or child abuse. Tests were ordered and a working diagnosis of a proximal radial head fracture with Type I OI was made based on the patient's history of multiple fractures and the father's history of fractures. Treatment options and counseling were discussed, including referral to physical therapy and a geneticist.
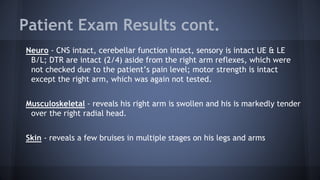
![Acute Fracture observed in OI
Frontal radiograph of the leg
in a patient with osteogenesis
imperfecta (OI)
Hypertrophic callus formation
six weeks after femoral shaft
fracture at age 9 month
A). A radiograph taken 1.5 yr
later shows remodeling of the
callus
(B).multiple white bands
[zebra stripes] parallel to the
physis
(11)
Type I Osteogenesis
Imperfecta, Acute fracture
observed in the radius and
ulna. Old healing humeral
fracture with callus
formation is observed.](https://image.slidesharecdn.com/osteogenesisimperfecta-150726140655-lva1-app6891/85/Osteogenesis-imperfecta-10-320.jpg)