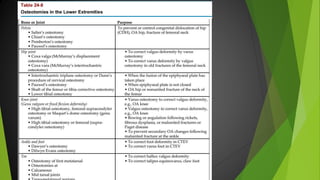
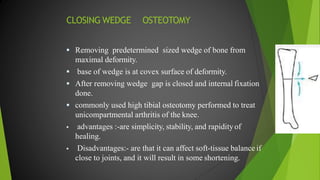
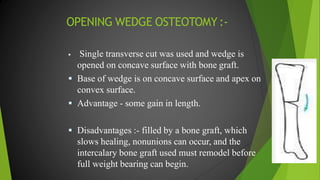
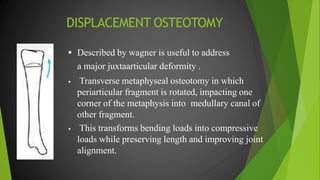
Osteotomy is a surgical procedure that cuts or divides bone to improve the function of a limb or provide stability to a joint. It involves three stages - dividing the bone, immobilizing it to allow correction and realignment, and physiotherapy to restore full function. Different types of osteotomies like closing wedge, opening wedge, and oblique cuts are used to correct various bone deformities and dysfunctions. Post-surgery physiotherapy focuses on reducing pain and swelling, maintaining stability, and gradually improving range of motion and strength. Complications can include under or overcorrection of deformity, nerve damage, compartment syndrome, and non-union of bone.