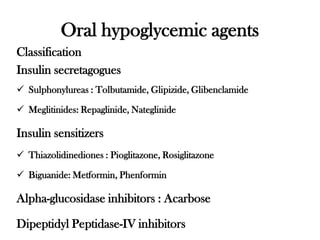
This document discusses various classes of oral hypoglycemic agents used to treat type 2 diabetes. It describes insulin secretagogues like sulfonylureas and meglitinides that promote insulin release from the pancreas. Insulin sensitizers like biguanides and thiazolidinediones lower blood sugar by improving insulin response in tissues without stimulating insulin secretion. Alpha-glucosidase inhibitors and DPP-IV inhibitors are also discussed along with their mechanisms of action and examples within each class. Side effects are provided for some of the drug classes.






![1-cyclohexyl-3-(4-[2-{5-methyl pyrazine carboxamide} ethyl] phenyl)sulfonyl urea
1-(4-methylcyclohexyl)-3-(4-[2-{3-ethyl-4-methyl-2-oxo) pyrrolidine carboxamide}
ethyl] phenyl)sulfonyl urea](https://image.slidesharecdn.com/oralhypoglycemicagent1-221126172857-f7ed37fe/85/Oral-Hypoglycemic-Agent-1-pdf-9-320.jpg)




![2-ethoxy-4-(2-[3-methyl-1-[2-piperidyl)phenyl]
butyl ]amino-2-oxoethyl benzoic acid
3-phenyl-2-[4-(1-methylethyl)cyclohexylcarbonyl) aminopropanoic
acid](https://image.slidesharecdn.com/oralhypoglycemicagent1-221126172857-f7ed37fe/85/Oral-Hypoglycemic-Agent-1-pdf-14-320.jpg)



![Pioglitazone/ 5-(4-(2-(4-ethylpyridin-2-yl)ethoxy) benzyl) thiazolidine-2,4-dione
Rosiglitazone/
5-[[4-[2-[N-methyl(pyridin-2-yl)amino]ethoxy]phenyl]methyl]-1,3-thiazolidine-2,4-dione
Side effects include Fluid retention, Weight gain, Hypoglycemia, Respiratory Tract Infection](https://image.slidesharecdn.com/oralhypoglycemicagent1-221126172857-f7ed37fe/85/Oral-Hypoglycemic-Agent-1-pdf-18-320.jpg)

