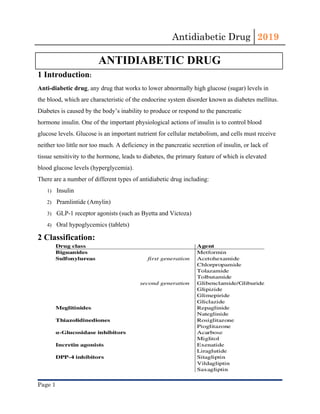
This document provides an overview of antidiabetic drugs, classifying them based on their mechanisms of action and summarizing their uses, side effects, and contraindications. The main classes described include biguanides (e.g. metformin), sulfonylureas, meglitinides, incretin mimetics, DPP-4 inhibitors, SGLT-2 inhibitors, alpha-glucosidase inhibitors, and thiazolidinediones. Metformin is noted as the first-line oral medication for type 2 diabetes due to its efficacy, safety profile, and cost-effectiveness. All antidiabetic drugs require careful consideration of risks like hypoglycemia and drug interactions when prescribing based on a















![Antidiabetic Drug 2019
References:
1. https://www.amboss.com/us/knowledge/Antidiabetic_drugs
2. American Diabetes Association. Diabetes Basics. Accessed 11/5/2018
3. MIMS. 2013. [12 December 2013]. Available from: http://www.mims.co.uk/
Page 17](https://image.slidesharecdn.com/antidiabetic-drug-1-190517142411/85/Antidiabetic-drug-1-17-320.jpg)