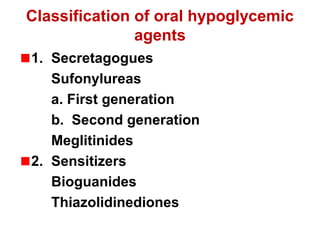
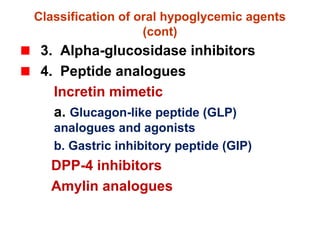
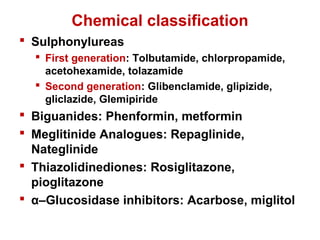
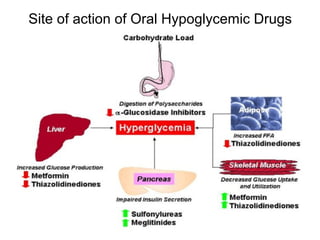
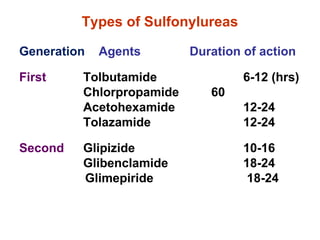
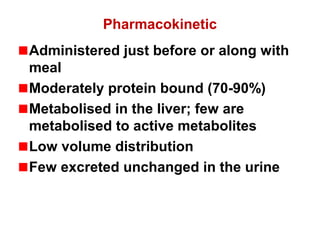
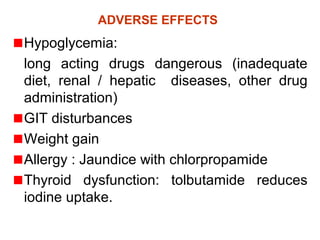
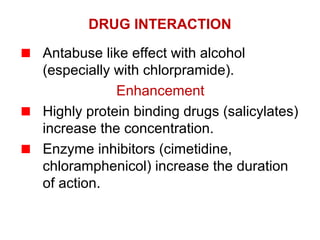
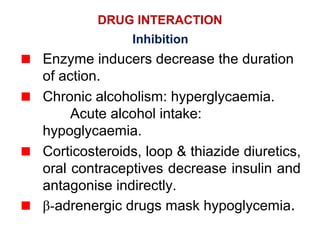
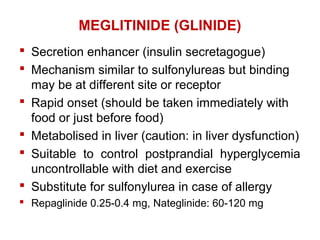
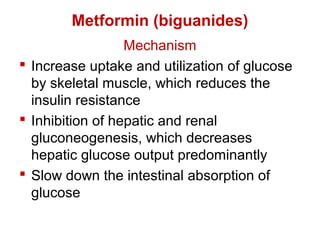
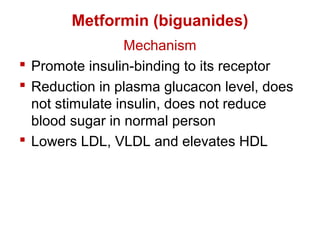
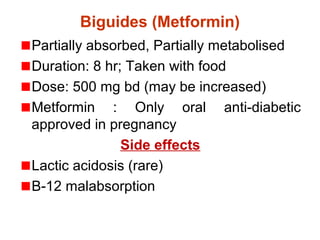
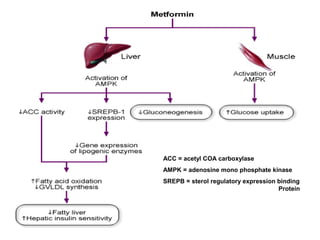
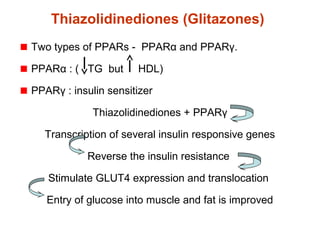
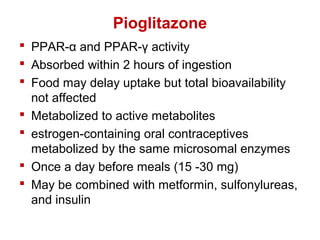
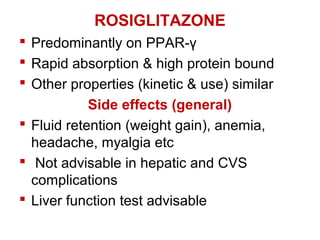
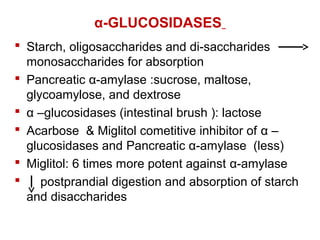
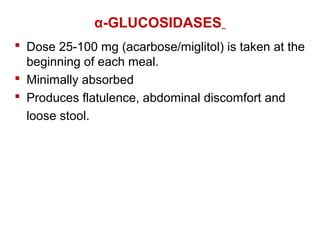
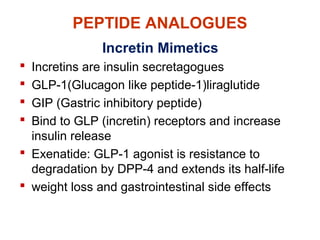
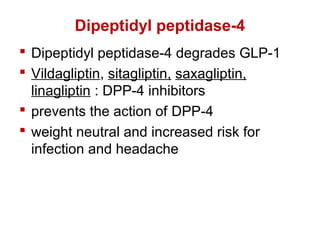
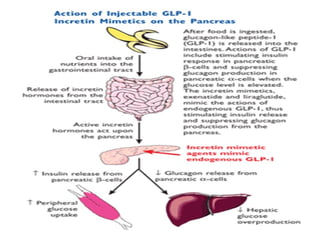
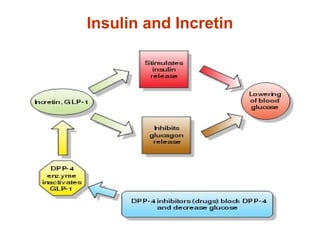
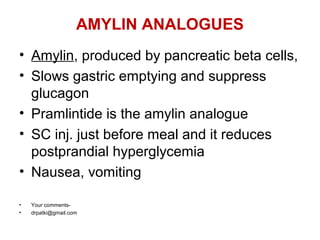
The document provides a comprehensive overview of oral hypoglycemic agents used in diabetes management, classifying them into categories such as secretagogues, sensitizers, and others. It details the mechanisms, pharmacokinetics, and side effects of different drug classes including sulfonylureas, biguanides like metformin, thiazolidinediones, and alpha-glucosidase inhibitors. Additionally, it discusses the roles of incretin mimetics and amylin analogues in enhancing insulin secretion and managing blood glucose levels.