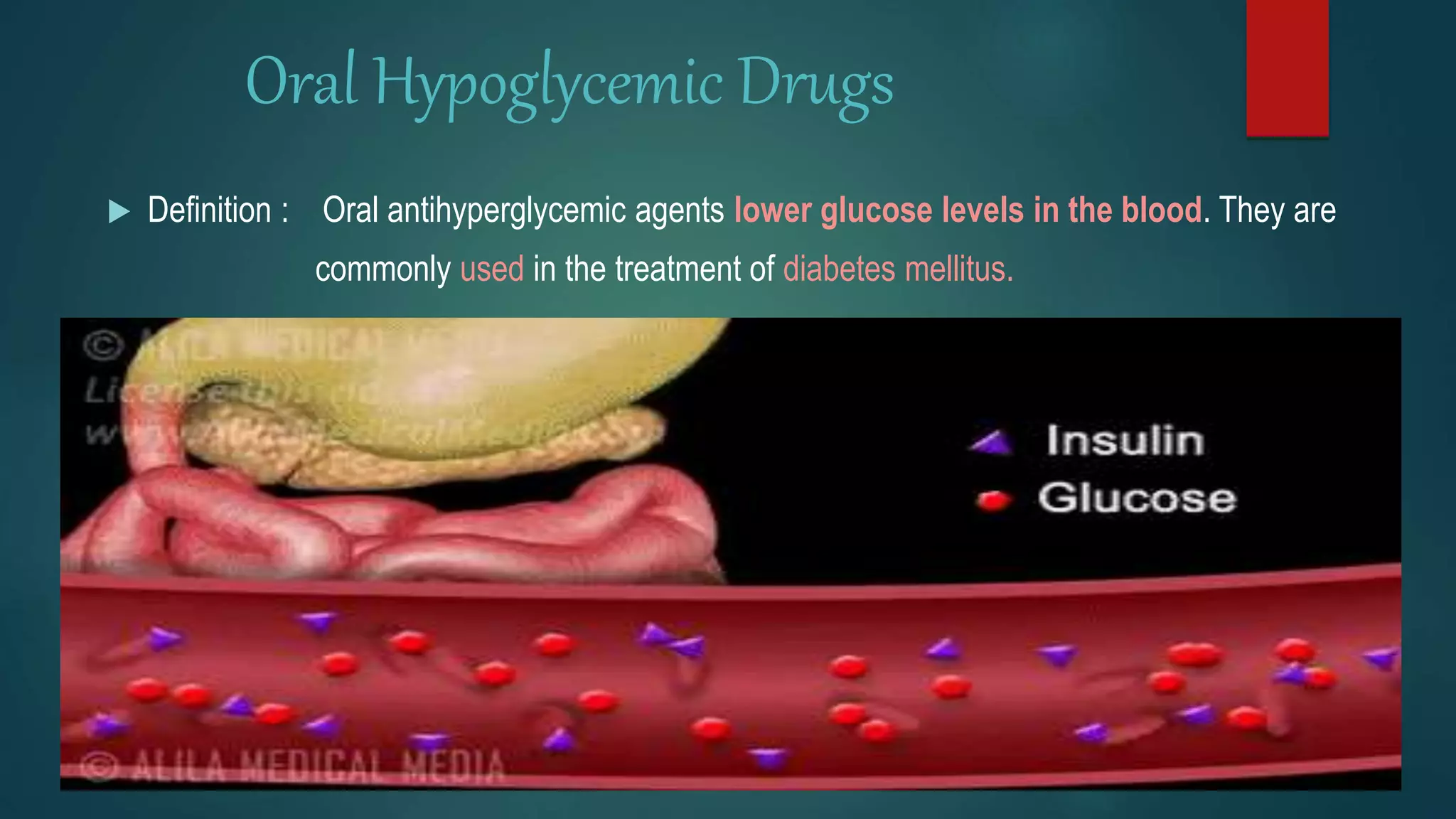
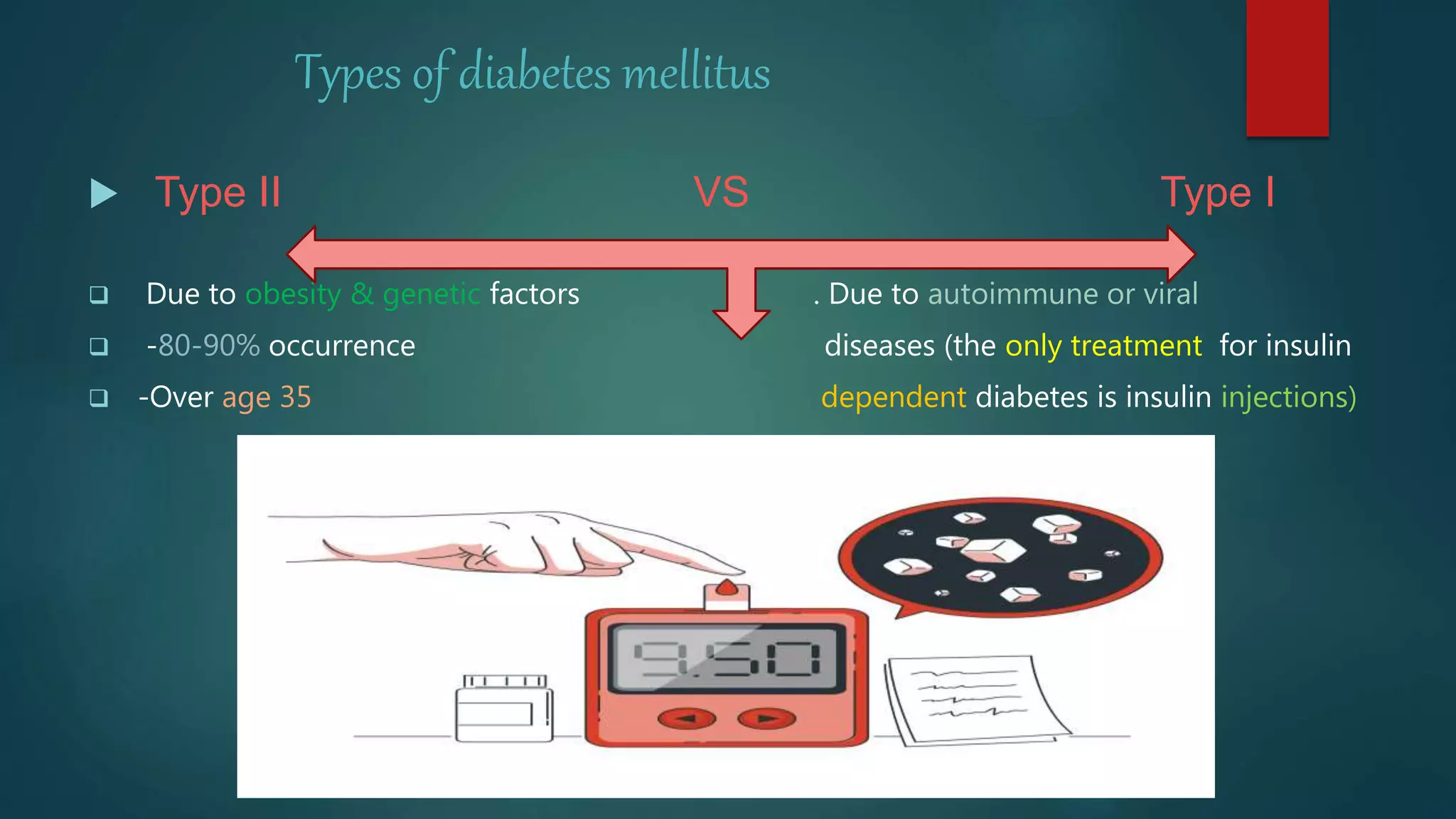
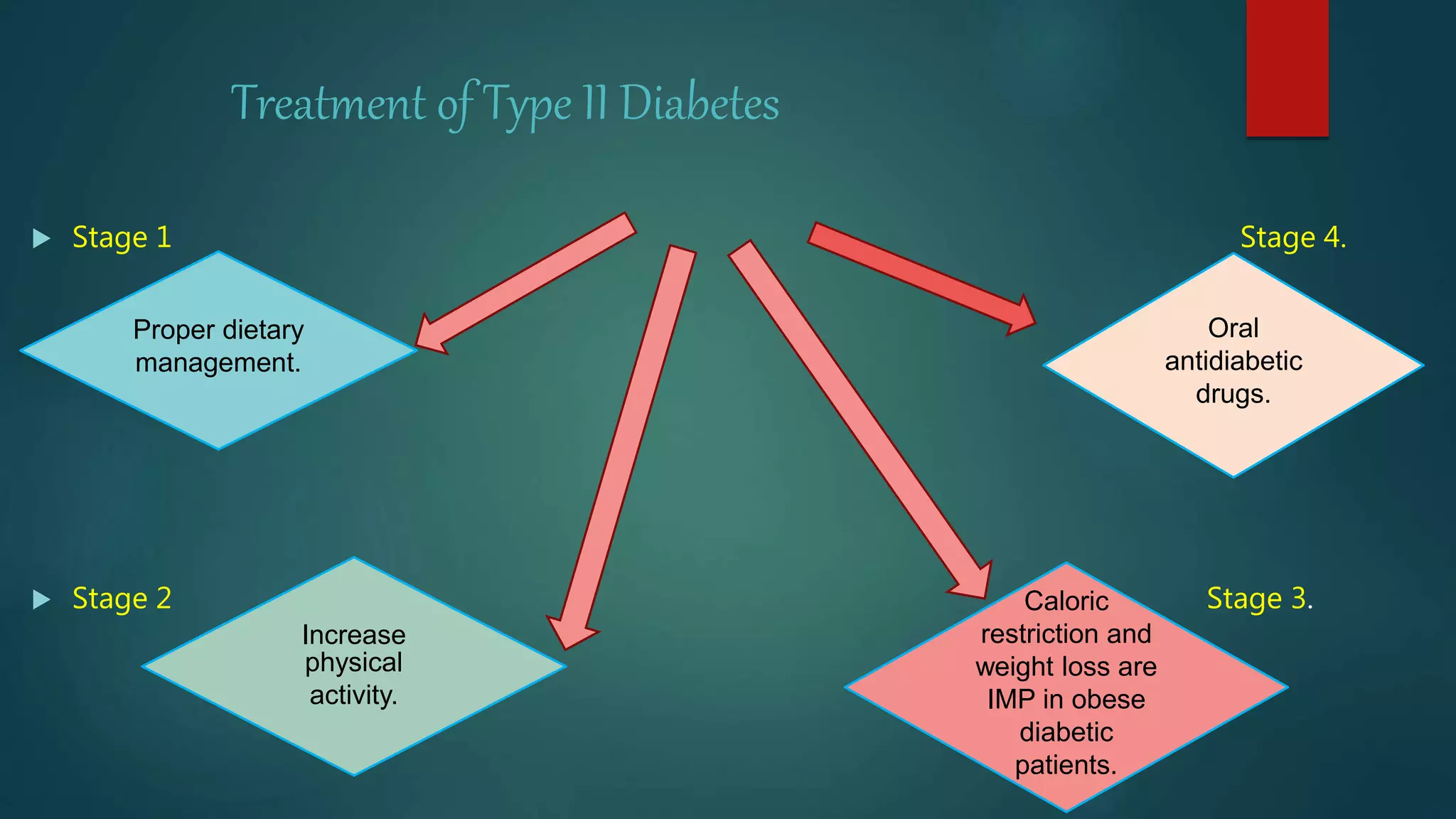
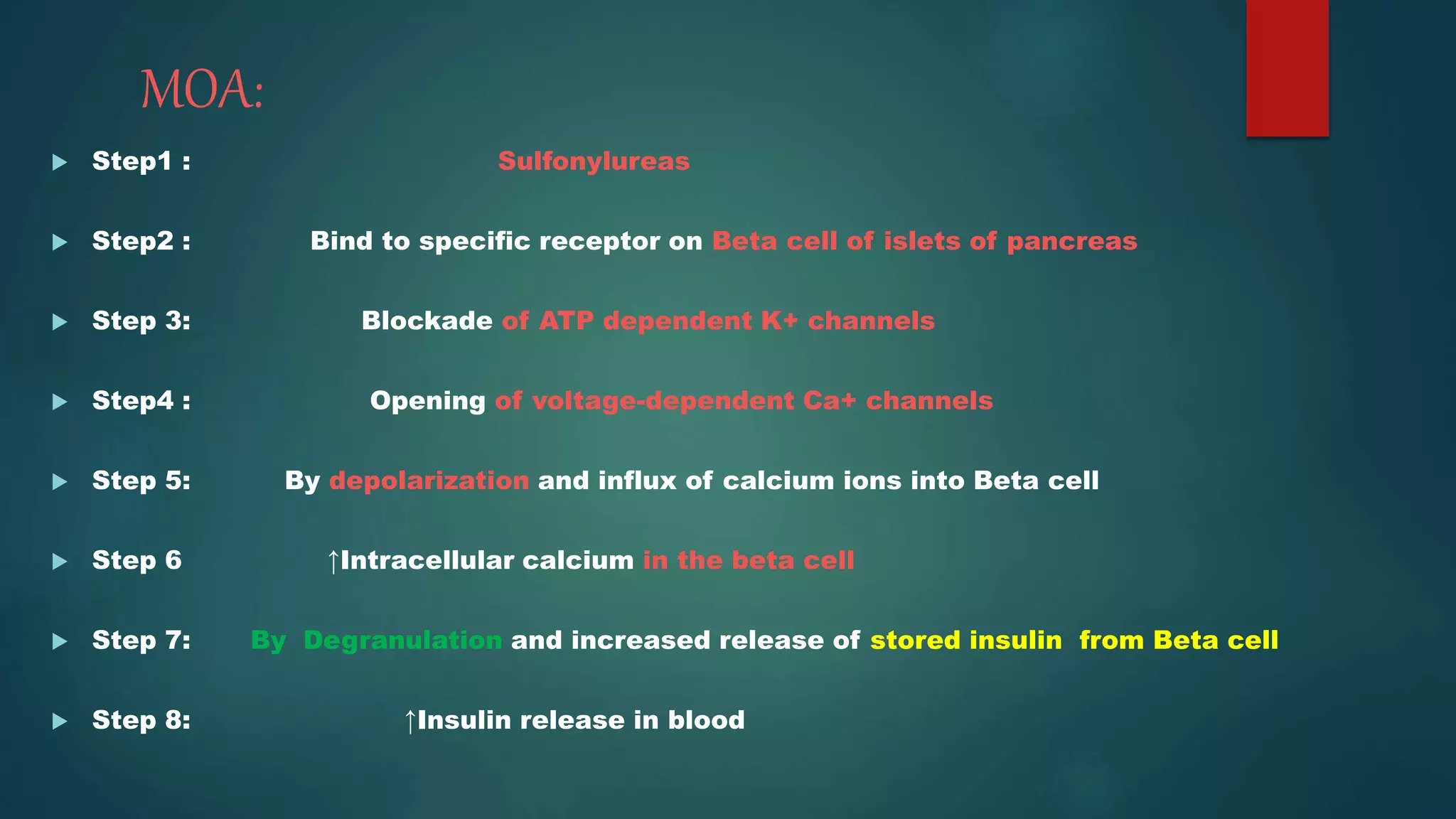
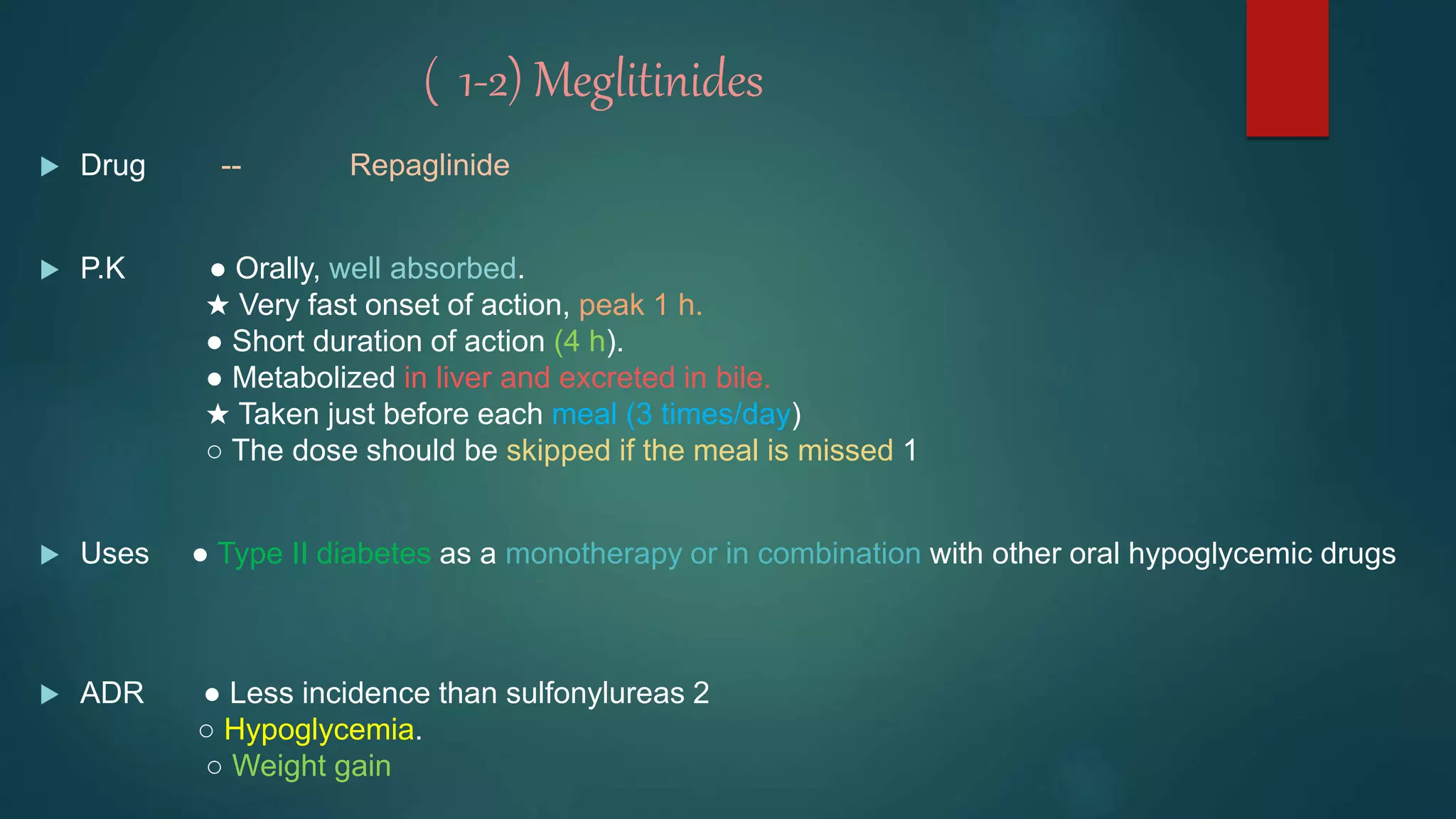
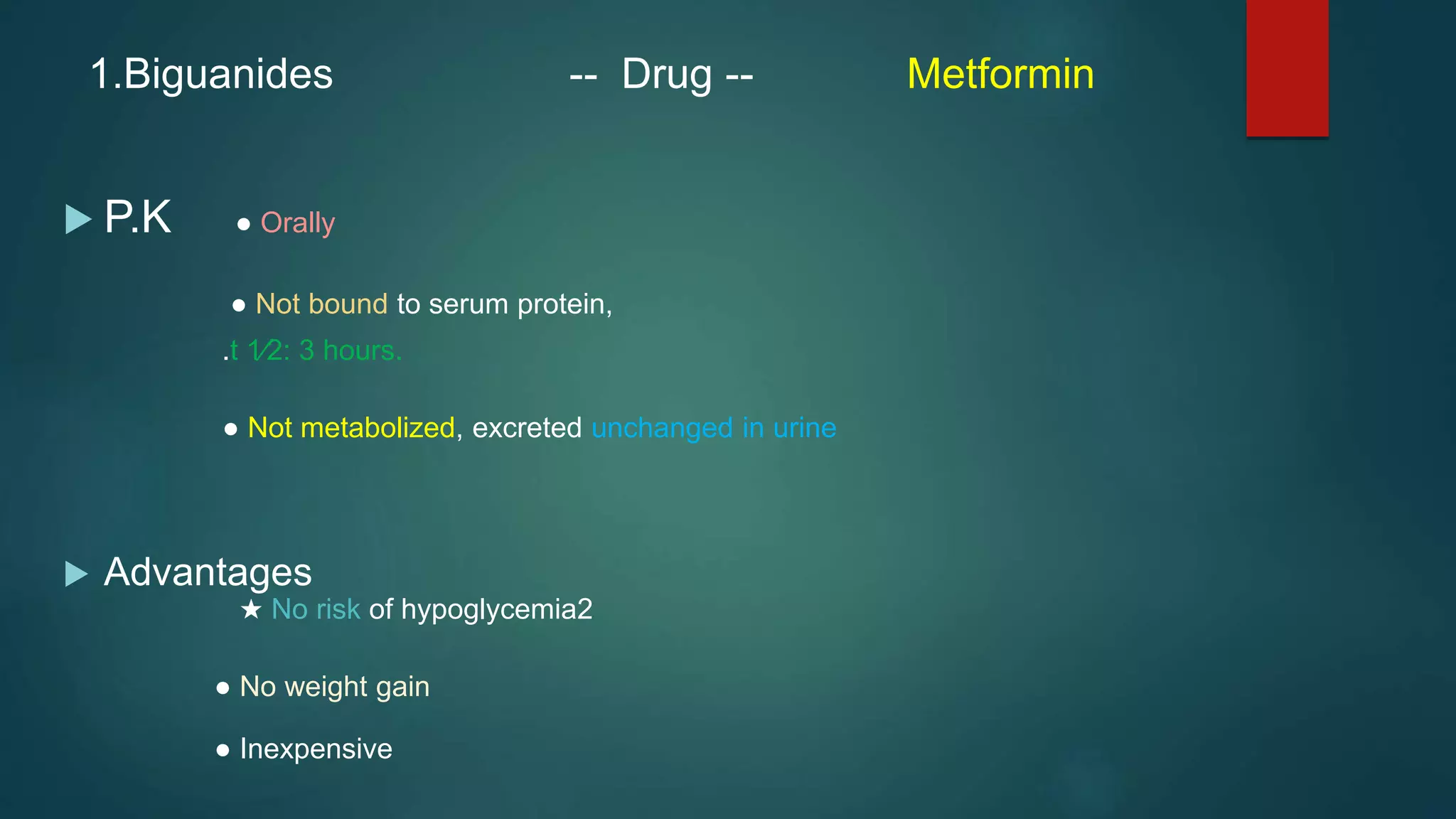
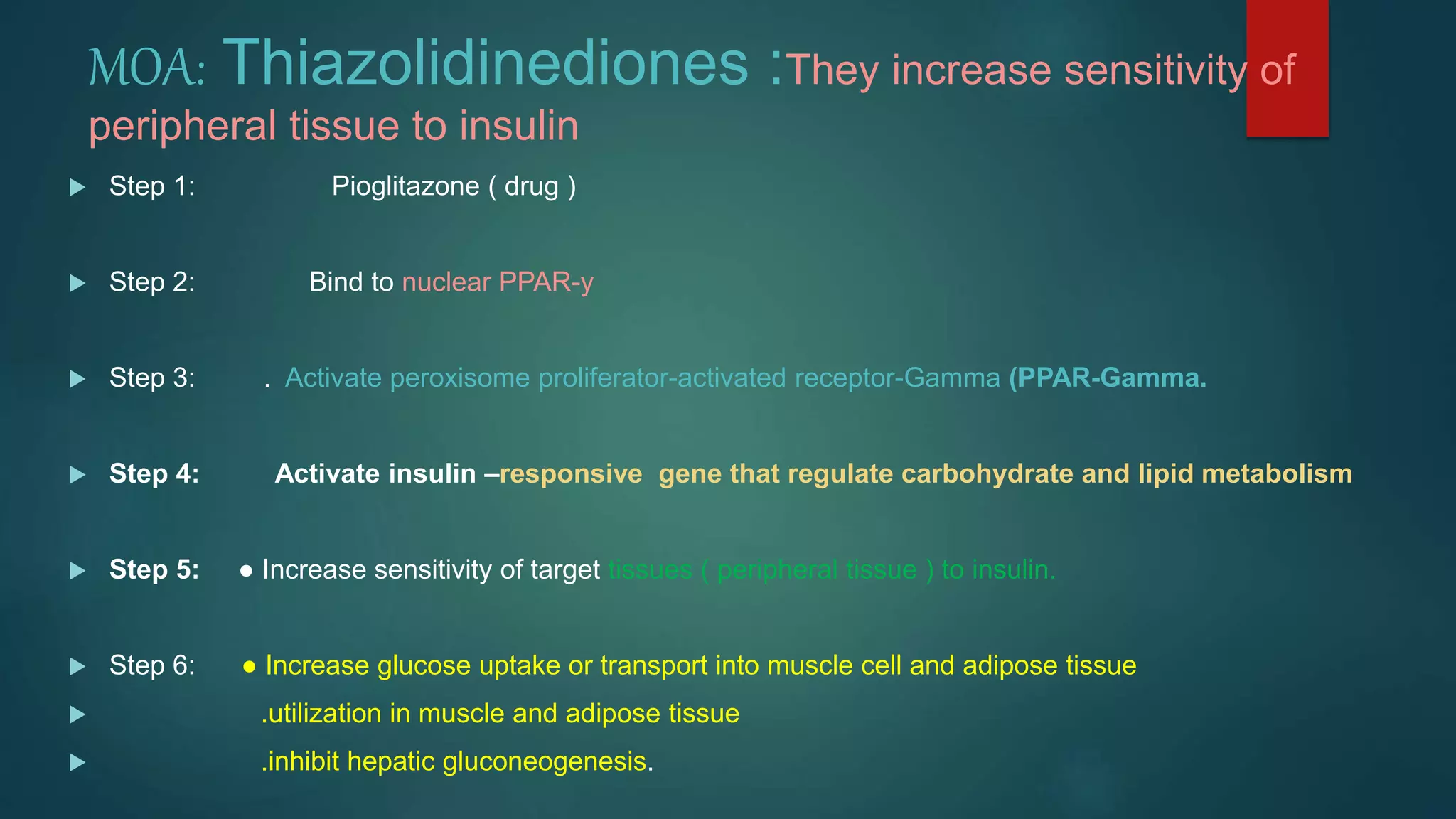
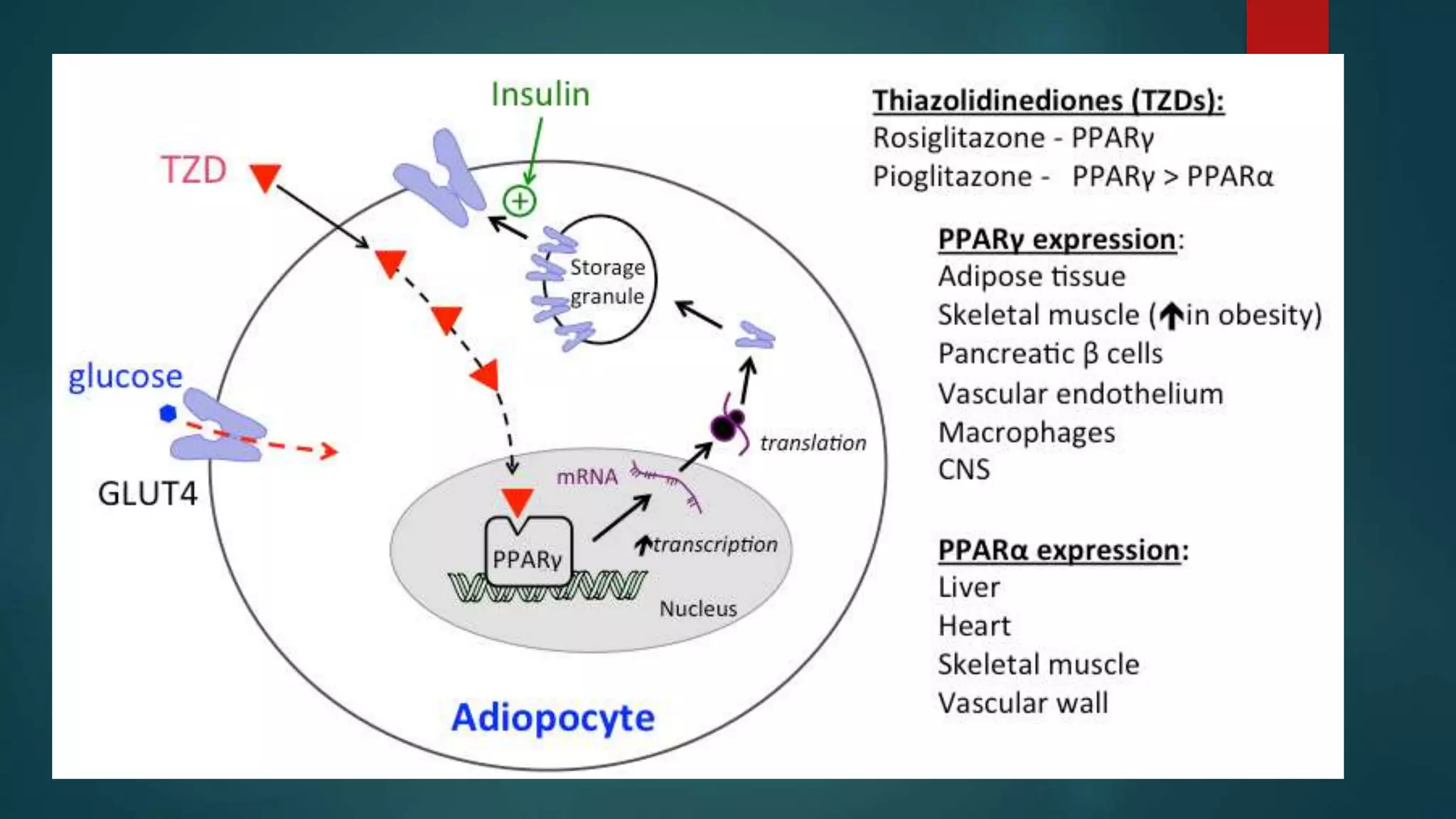
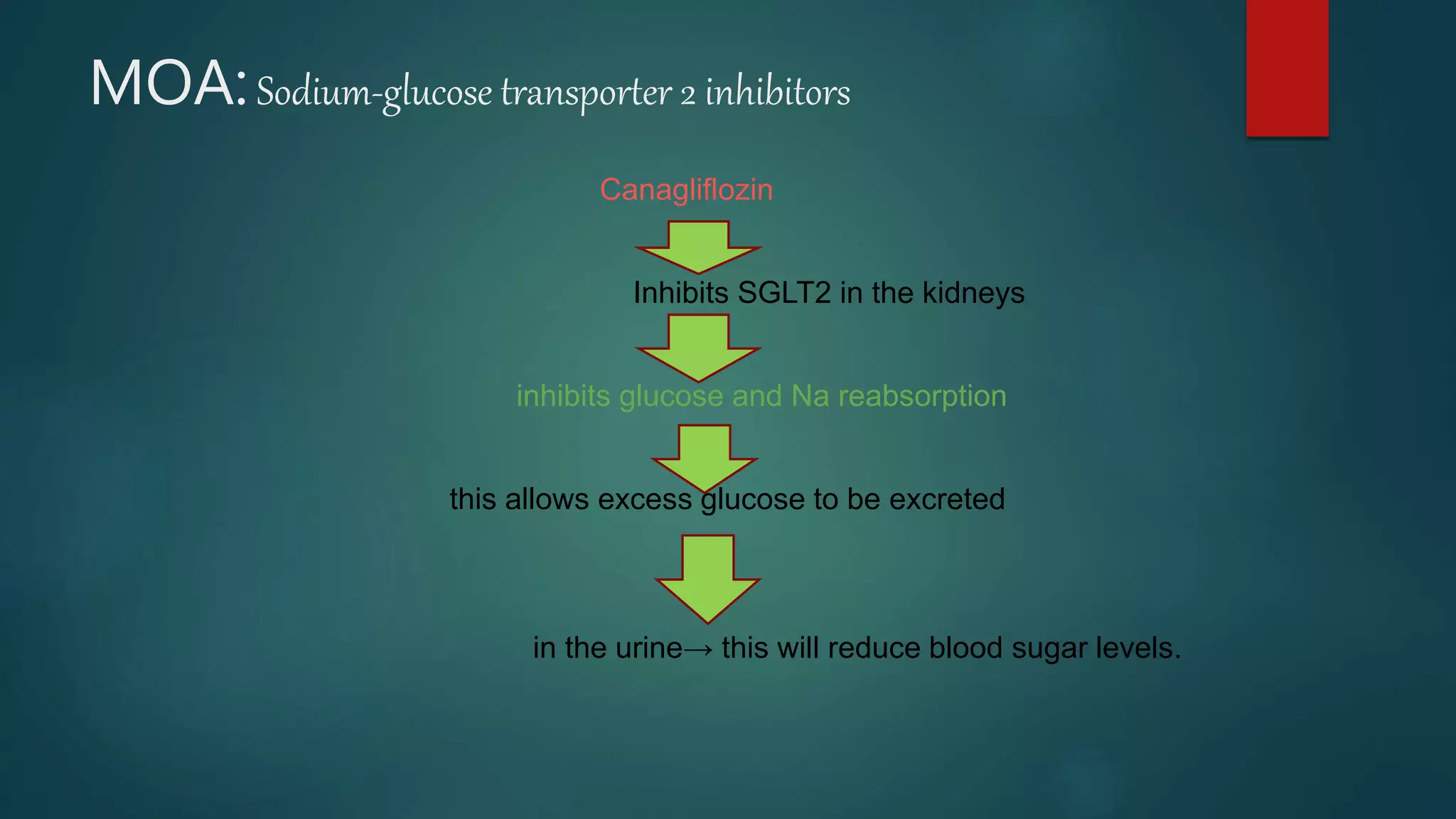
The document discusses oral hypoglycemic drugs, which are used to treat diabetes mellitus by lowering blood glucose levels. It classifies various antidiabetic medications, detailing their mechanisms of action, pharmacokinetics, clinical uses, and side effects, focusing on categories such as insulin secretagogues, insulin sensitizers, α-glucosidase inhibitors, and sodium-glucose transporter 2 inhibitors. The treatment approach for type 2 diabetes follows a stepwise method, involving diet, exercise, and medications, with a focus on individualized patient care.