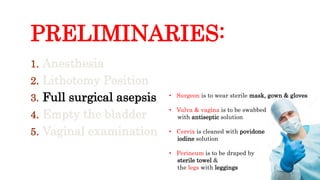
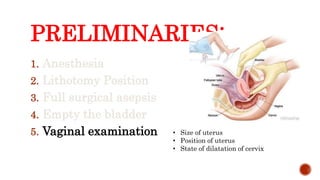
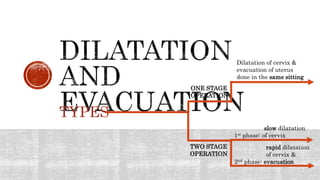
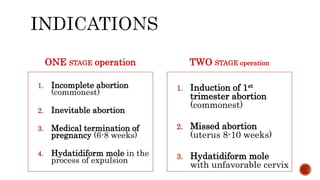
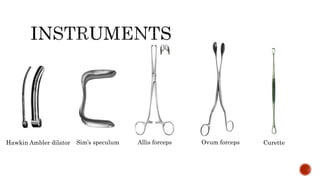
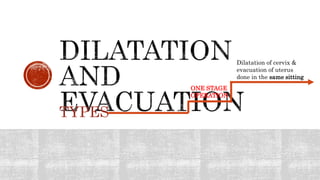
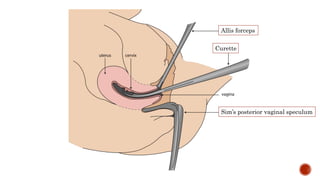
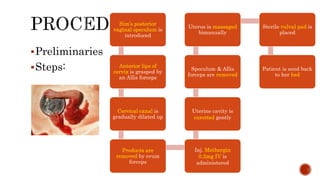
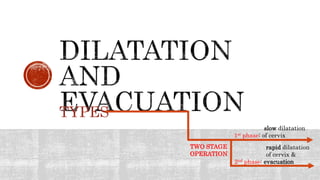
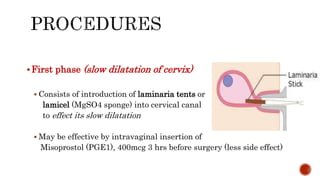
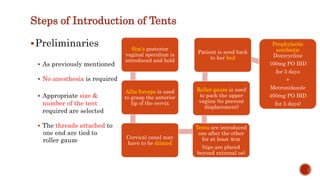
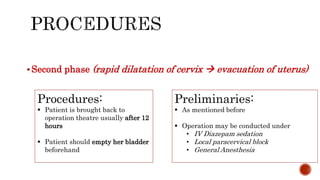
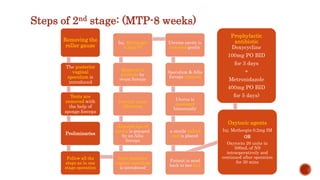
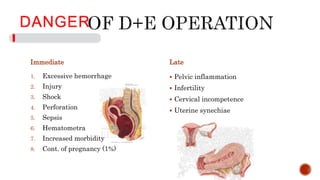
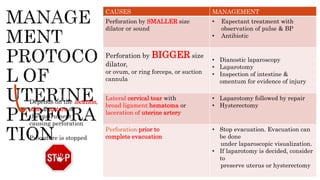
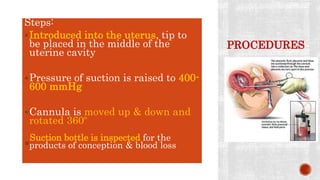
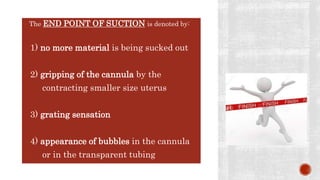
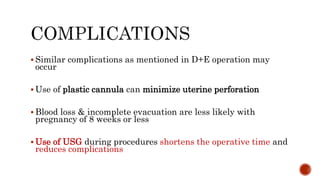
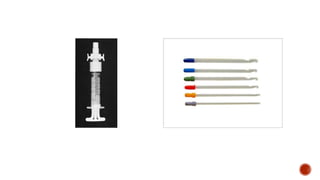
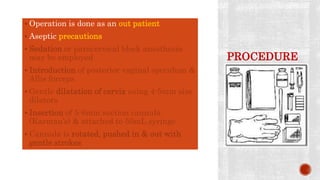
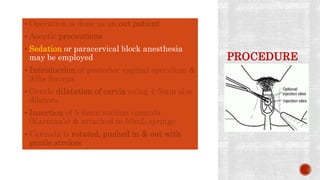
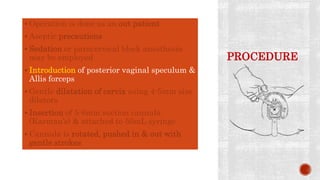
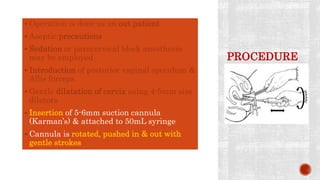
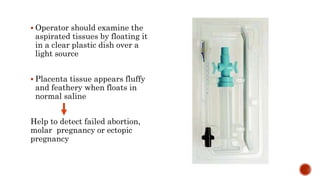
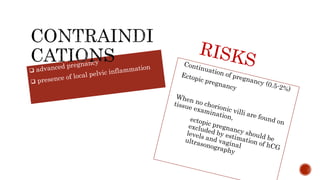
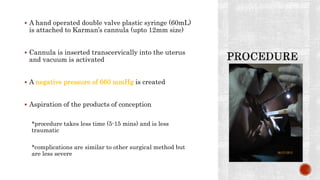
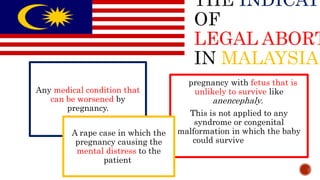
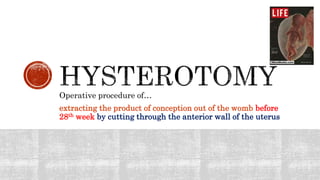
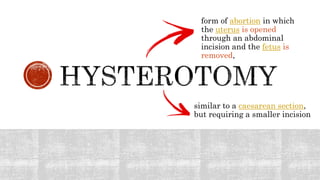
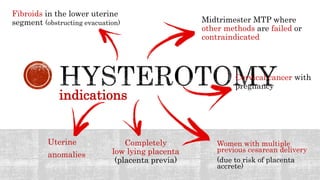
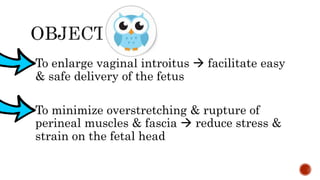
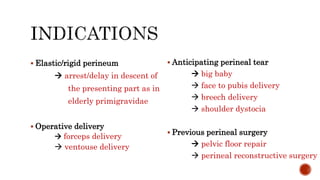
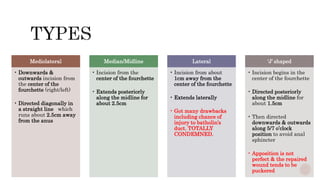
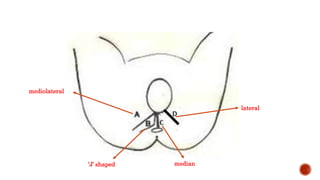
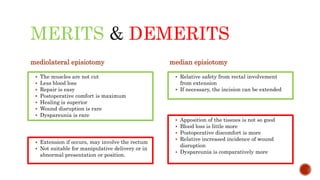
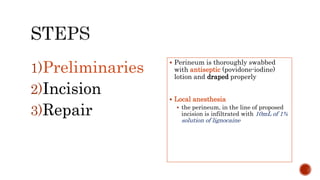
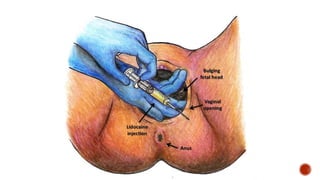
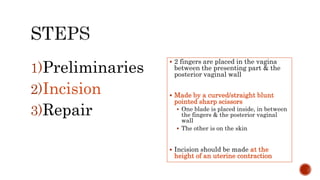
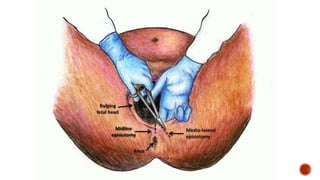
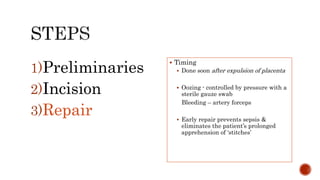
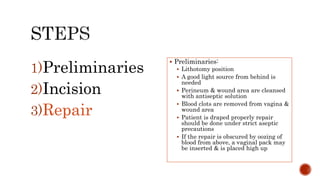
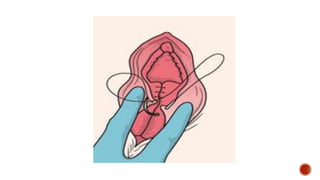
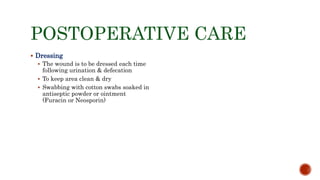
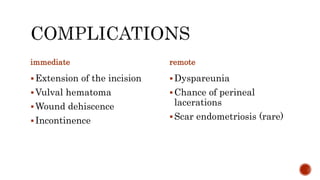
The document details various surgical procedures related to obstetrics and gynecology, including dilation and evacuation, suction evacuation, cesarean section, and episiotomy. It outlines surgical preliminaries, instruments, techniques, and potential complications associated with each procedure. Additionally, it discusses indications for interventions and postoperative care protocols.