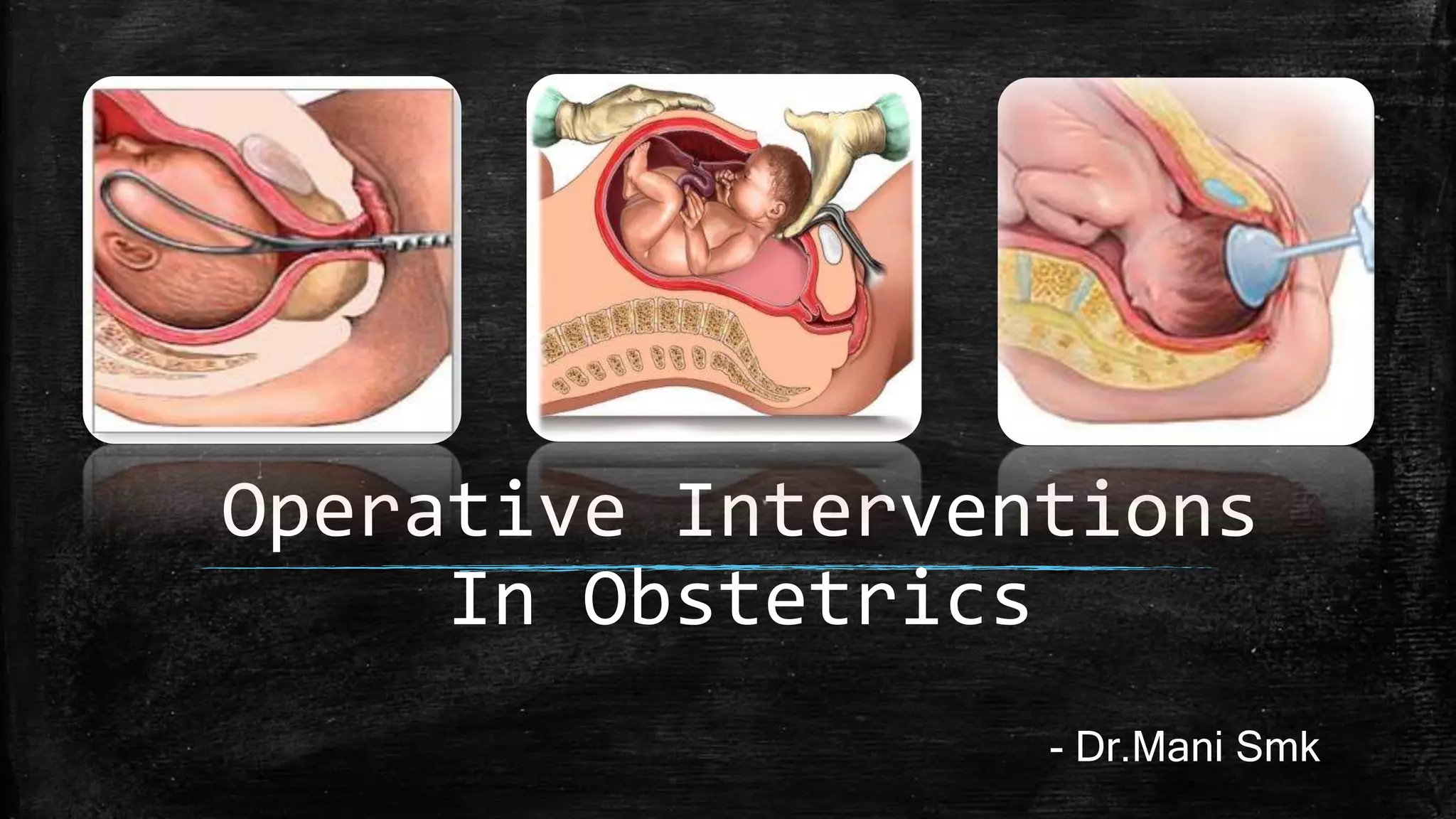
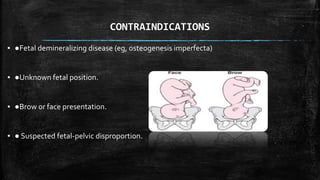
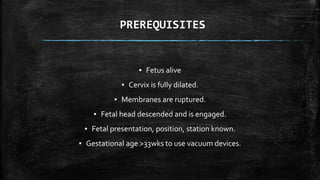
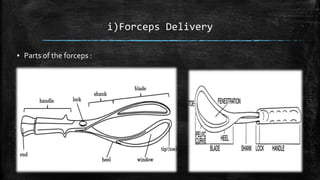
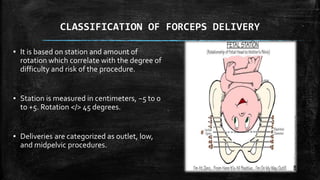
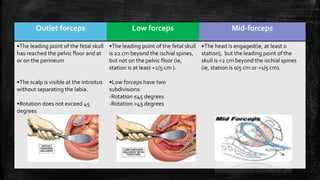
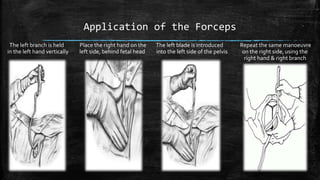
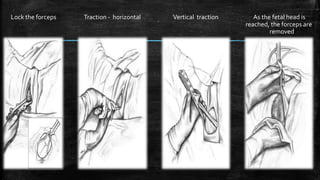
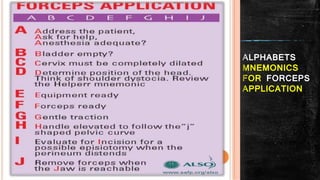
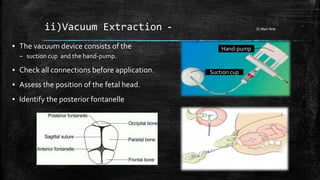
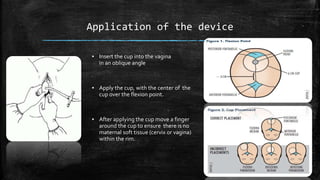
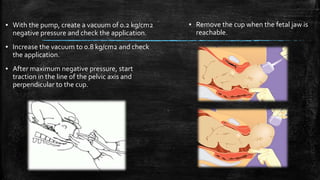
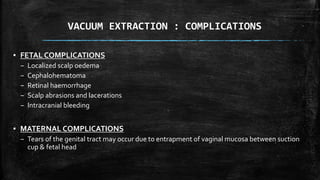
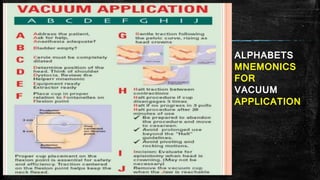
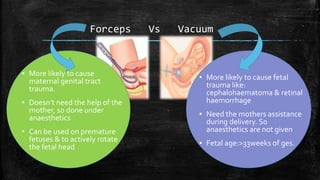
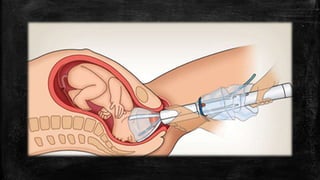
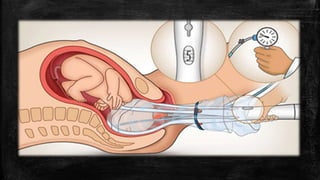
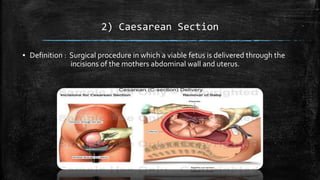
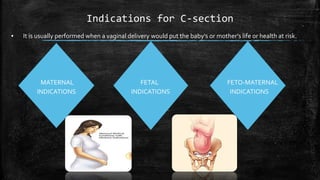
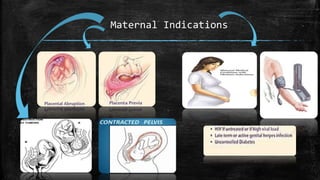
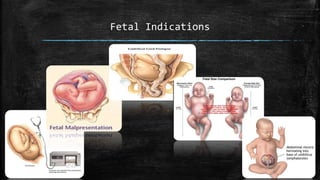
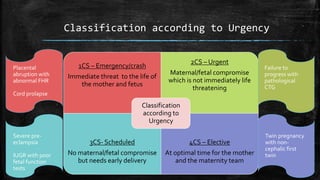
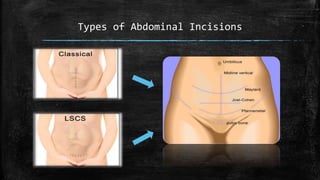
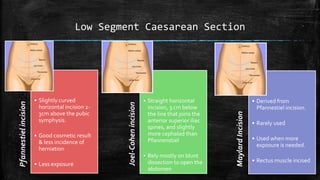
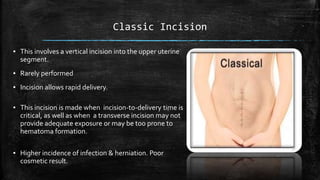
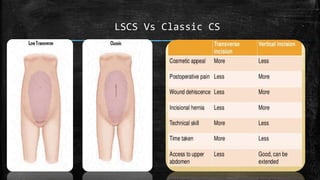
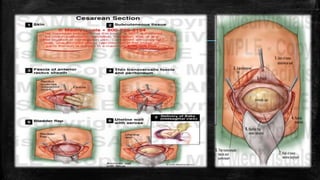
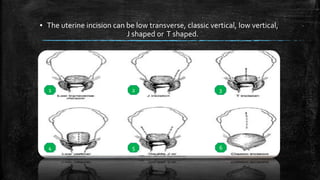
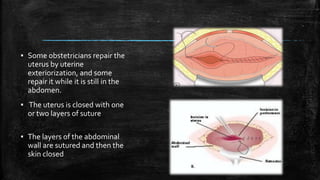
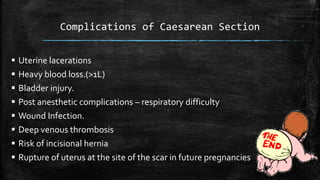
This document provides an overview of operative interventions in obstetrics, including operative vaginal delivery and caesarean section. It describes the indications, contraindications, prerequisites and techniques for operative vaginal delivery using forceps or vacuum extraction. The classifications, applications, and complications of forceps delivery are outlined. For vacuum extraction, the device components and application steps are explained. Caesarean section is defined and maternal, fetal, and fetomaternal indications listed. The document describes the classification of c-sections by urgency, types of abdominal incisions including low segment and classic, and the procedure steps. Complications of c-section are also summarized.