This document provides information about hysteroscopy, including:
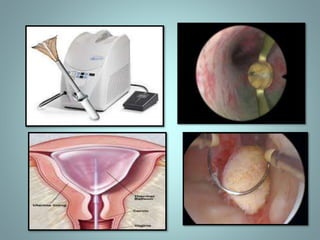
- A hysteroscope is an endoscope used to visualize the uterine cavity and perform procedures.
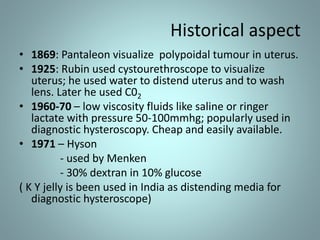
- It describes the historical development of hysteroscopy from the 19th century to modern techniques.
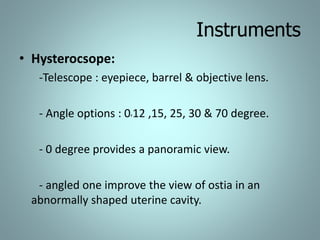
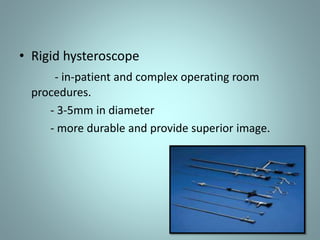
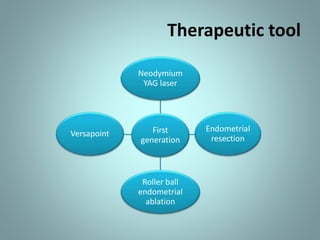
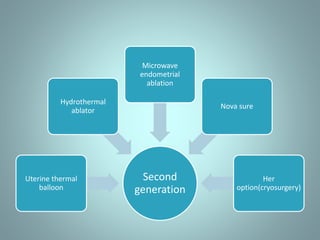
- The types of hysteroscopes and instrumentation used are outlined, including distention media, electrodes, sheaths, and cameras.
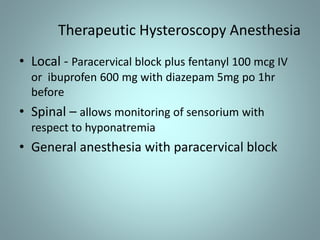
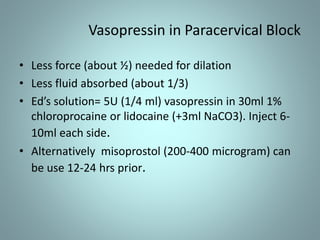
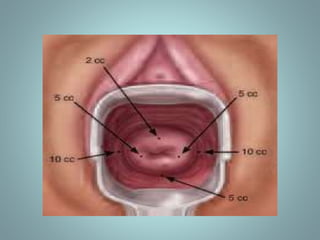
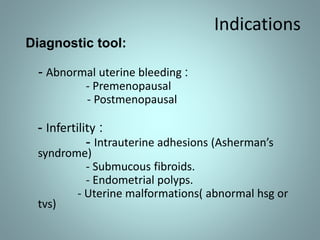
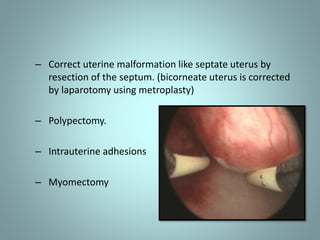
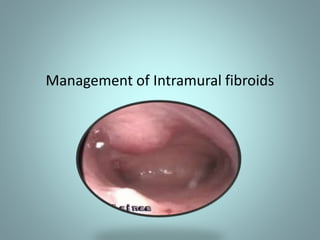
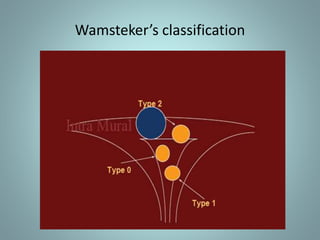
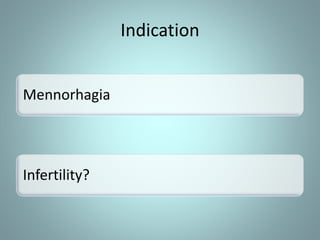
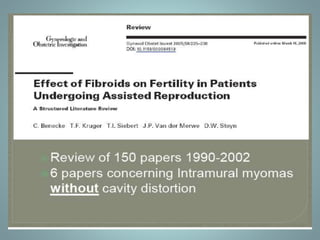
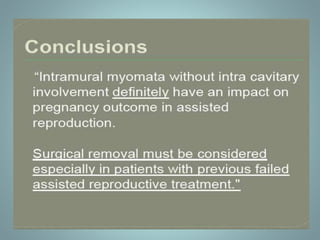
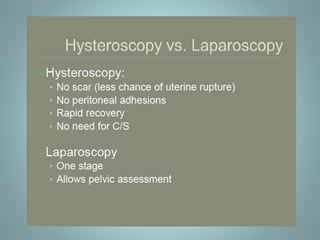
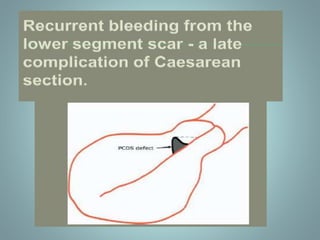
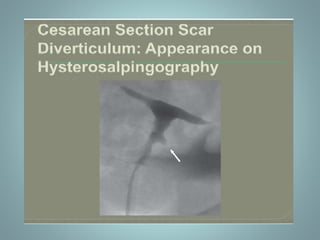
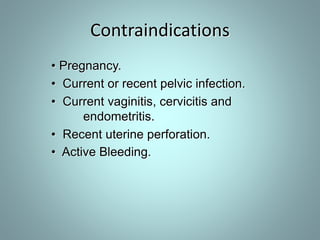
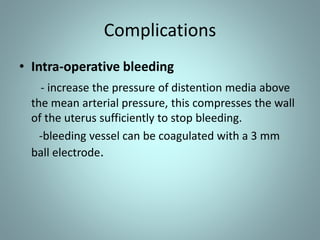
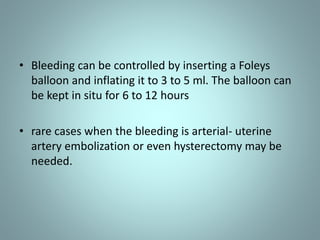
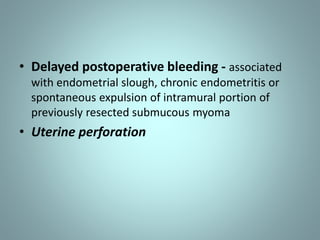
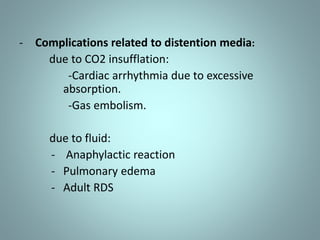
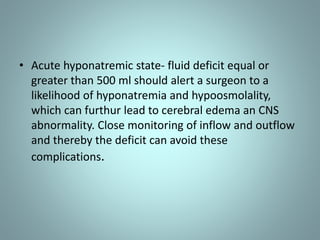
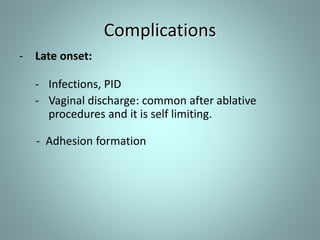
- The document discusses the procedures, indications, contraindications and complications of diagnostic and operative hysteroscopy.