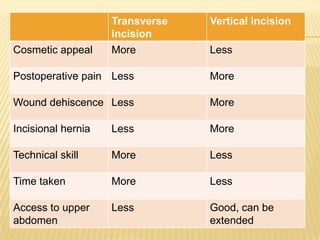
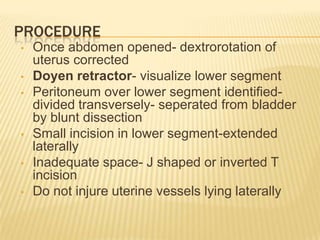
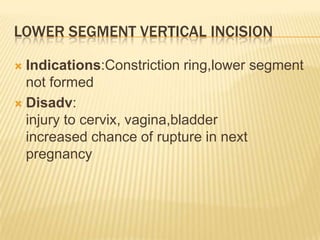
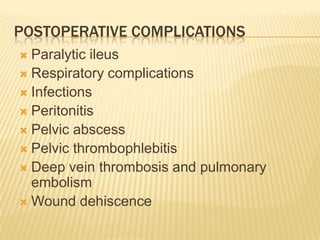
Caesarean section is the delivery of a fetus through an incision made in the mother's abdomen and uterus. It was originally a fatal operation but is now commonly performed worldwide. The WHO recommends an ideal c-section rate of 15-20% though rates have increased due to factors like previous c-sections and increased fetal distress diagnosis. C-sections are performed under spinal or epidural anesthesia with various abdominal incision types closed afterwards. Complications can include hemorrhage, infection, and injury to internal organs during the operation or issues like ileus, DVT and wound separation after.