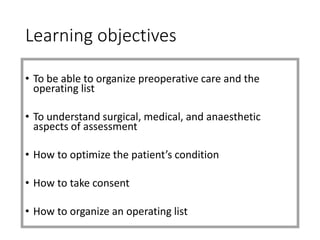
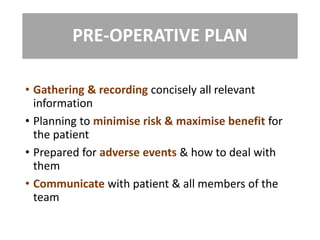
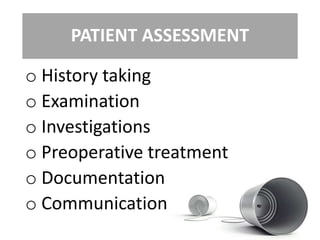
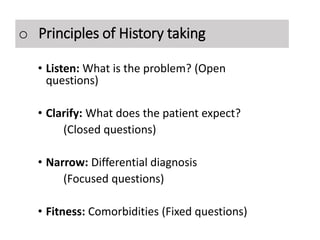
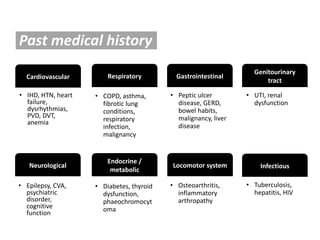
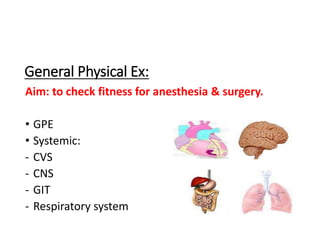
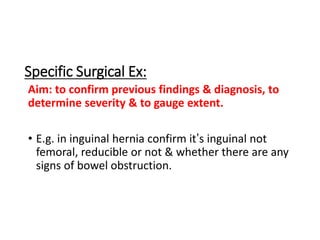
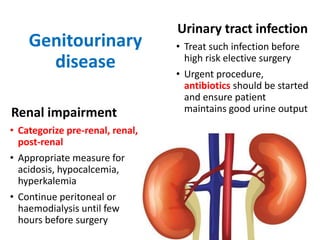
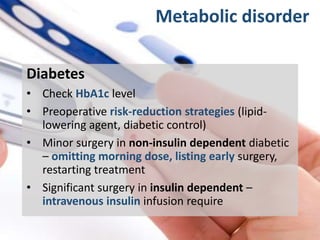
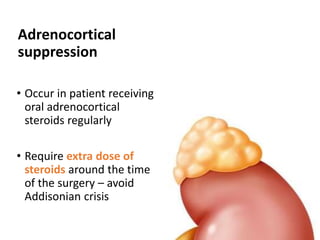
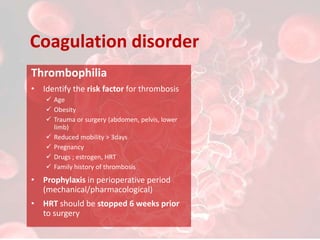
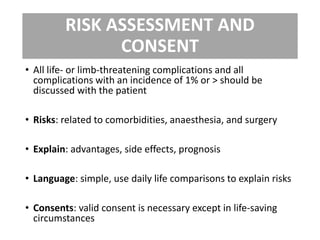
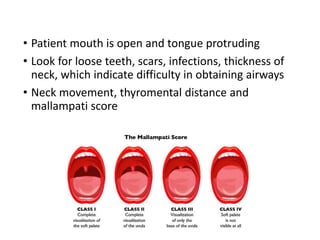
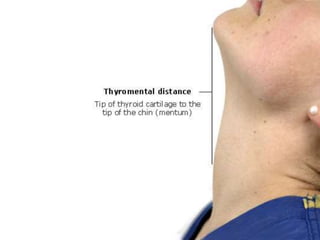
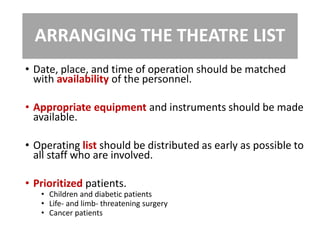
This document provides guidance on preoperative care and assessment. It outlines the objectives of preoperative care, which include organizing care and the operating list, understanding surgical, medical and anesthetic assessments, optimizing the patient's condition, obtaining consent, and organizing the operating list. It describes evaluating the patient's history, examination, investigations, preoperative conditions and treatment, and documenting the assessments. Key areas of focus for the patient assessment include cardiovascular, respiratory, gastrointestinal, genitourinary, neurological, endocrine and metabolic conditions. The document provides guidance on identifying and managing preoperative problems, obtaining informed consent, conducting a pre-anesthetic airway assessment, and arranging the operating theater list.