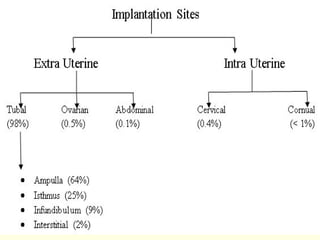
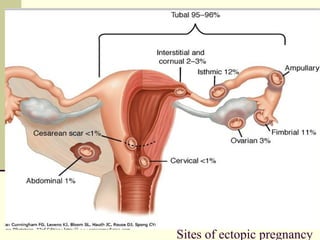
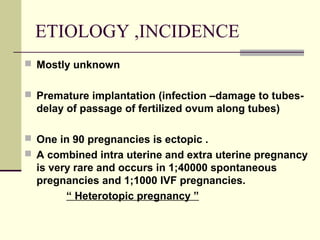
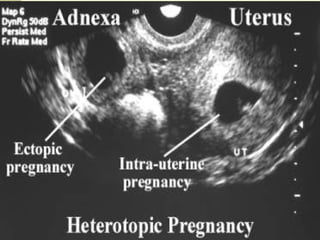
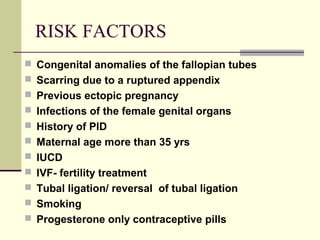
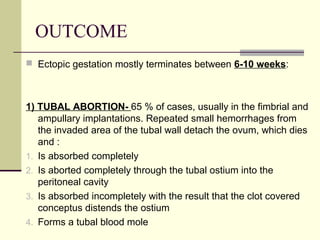
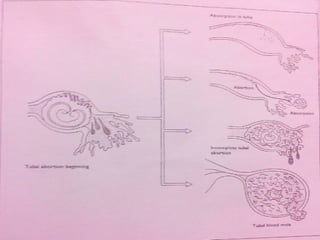
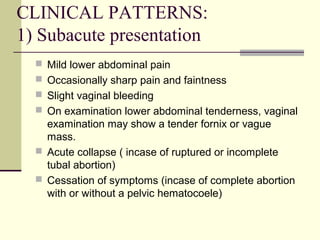
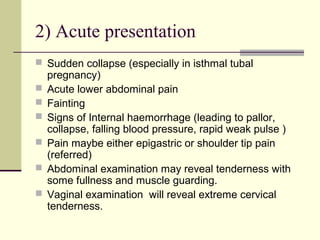
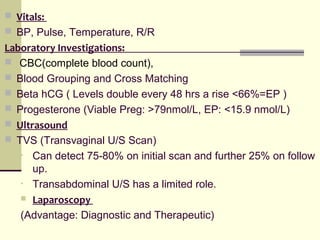
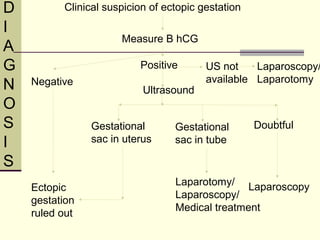
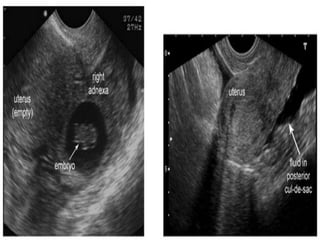
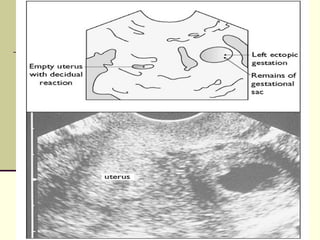
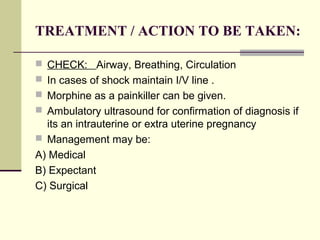
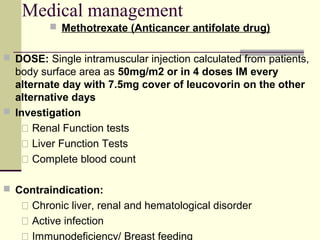
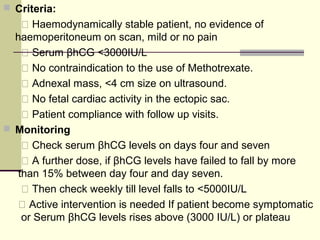
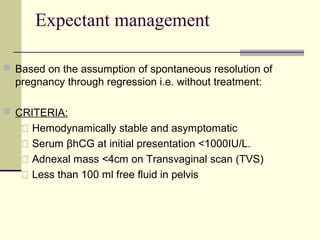
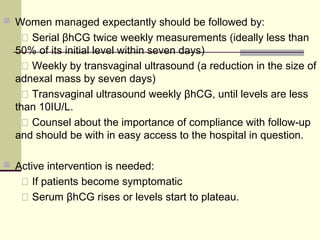
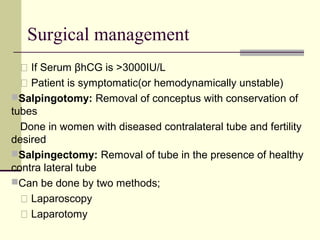
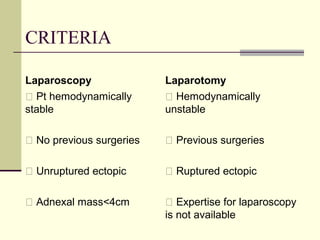
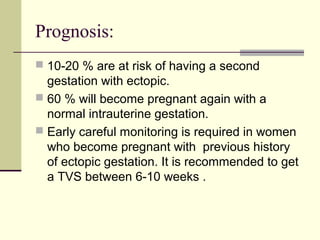
An ectopic pregnancy occurs when a fertilized egg implants outside of the uterus, usually in the fallopian tubes. Risk factors include previous ectopic pregnancy, infections, scarring of the fallopian tubes, and fertility treatments. Ectopic pregnancies can cause life-threatening bleeding if not treated properly. Diagnosis involves beta-hCG levels and ultrasound imaging. Treatment options include medication with methotrexate, expectant management with close monitoring, or surgery depending on the stability of the patient and characteristics of the ectopic pregnancy.