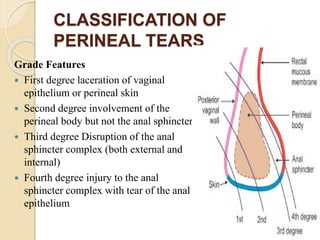
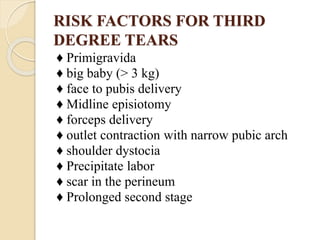
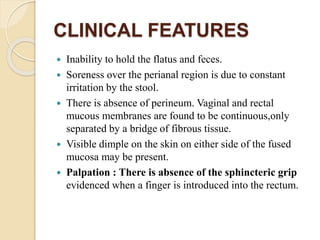
This document discusses various types of genital tract injuries including obstetric injuries from childbirth like complete perineal tears, as well as injuries from sexual assault, foreign bodies, trauma, and medical instrumentation. It outlines the definition, risk factors, clinical features, diagnosis, and treatment for conditions like complete perineal tears. Preventive measures during childbirth and operative repair techniques are described. Management of injuries from rape, trauma, retained foreign bodies, and instrumentation is also covered.