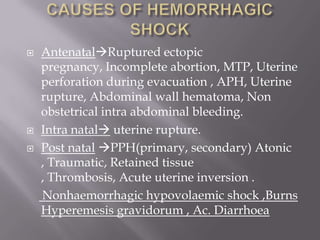
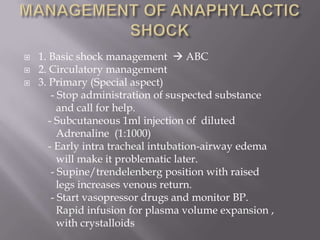
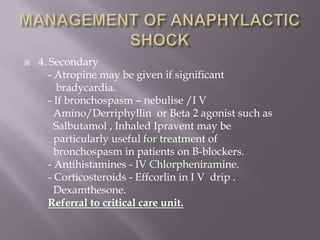
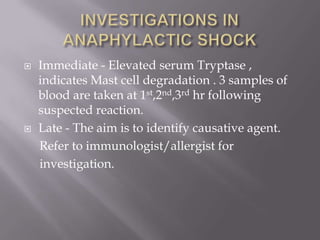
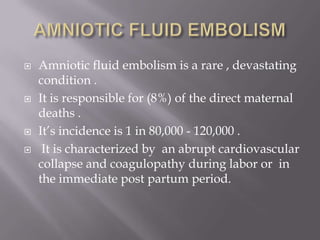
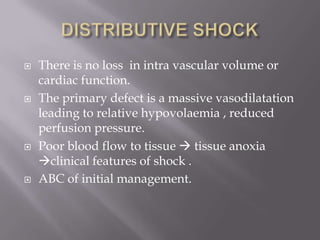
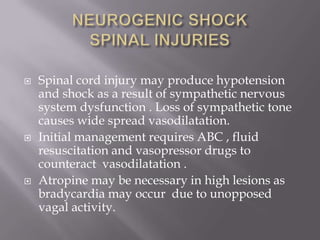
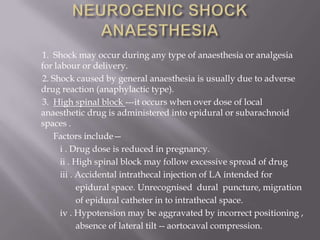
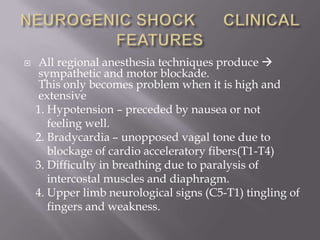
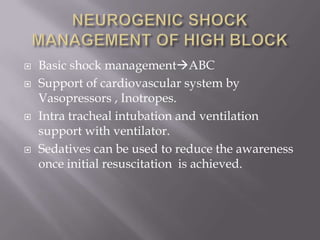
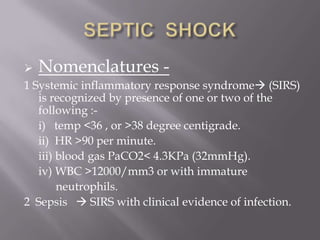
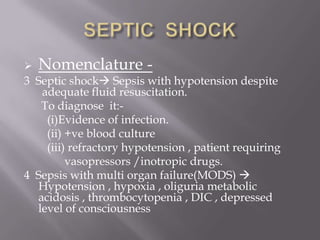
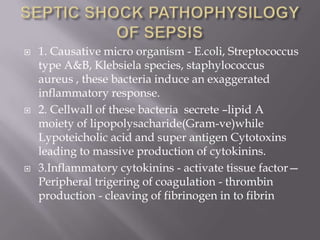
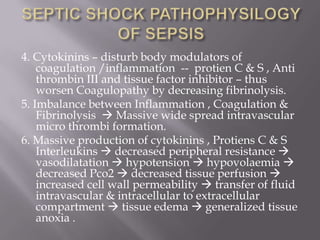
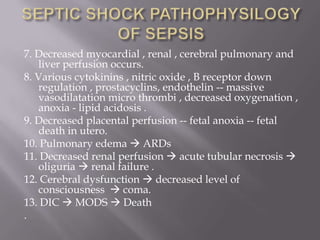
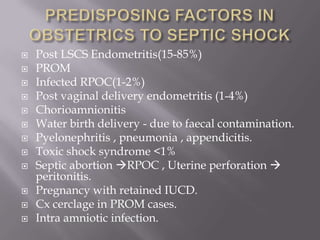
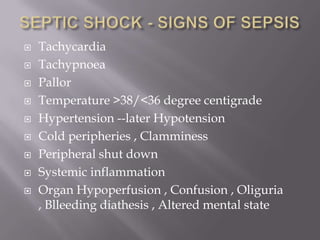
This document discusses obstetric shock, its causes, signs, stages, and management. Shock is a life-threatening medical emergency characterized by inadequate tissue perfusion and oxygenation. The major causes of obstetric shock are hemorrhage, sepsis, cardiogenic issues, neurogenic issues, and anaphylaxis. Untreated shock progresses through compensated, decompensated, and irreversible stages. Initial management focuses on airway, breathing, circulation, oxygenation, intravenous fluids, blood transfusion, and identifying and treating the underlying cause. Prompt recognition and treatment of obstetric shock can improve maternal and fetal outcomes.