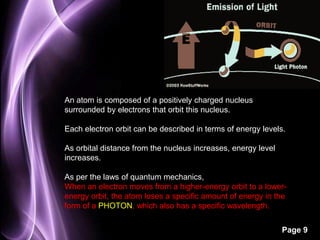
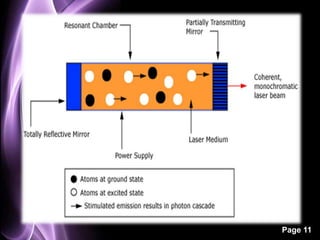
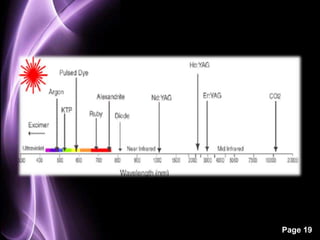
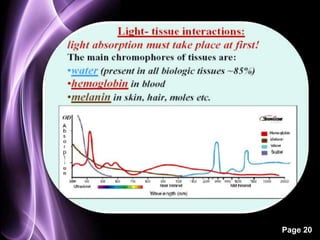
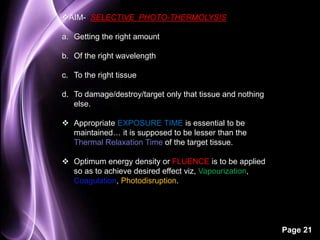
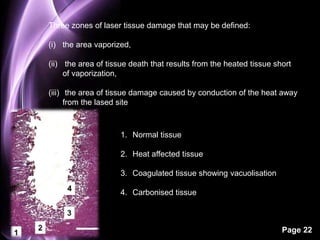
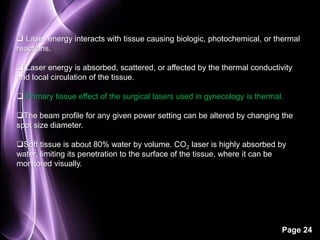
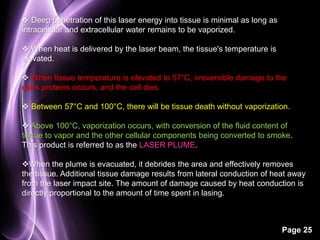
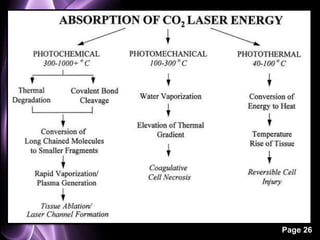
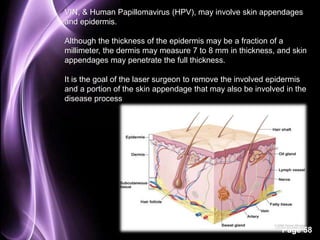
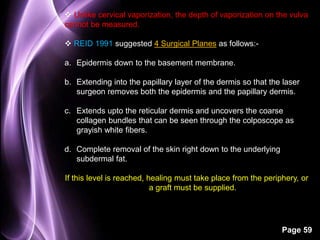
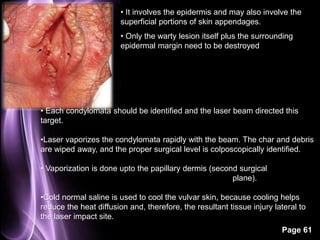
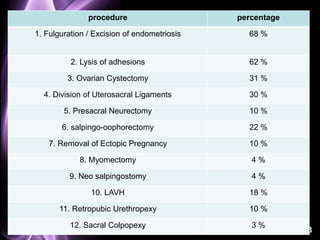
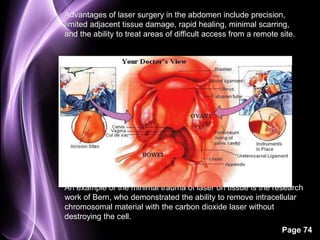
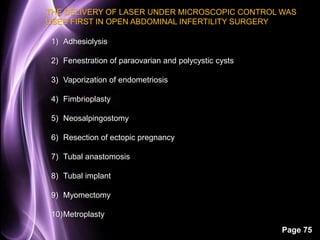
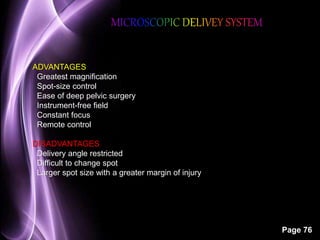
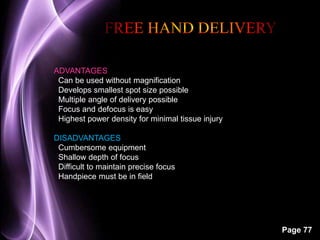
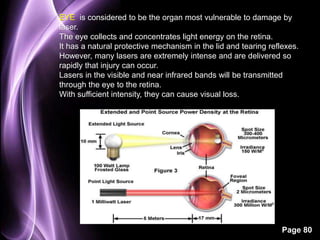
The document discusses lasers and their use in gynecology. It provides background on the history and development of lasers, including how they work using stimulated emission and have properties of monochromaticity, directionality, coherence, and a quantum nature. It then discusses the specific applications and effects of lasers in gynecological surgery, noting they are useful surgical tools but require carefully designed studies to understand long-term benefits. Lasers can be used to vaporize, coagulate, or photodisrupt tissue depending on the energy density or fluence applied.