1. Subinvolution, breast engorgement, mastitis, breast abscess, and thrombophlebitis are common postpartum complications that can occur.
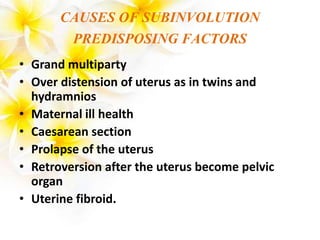
2. Subinvolution occurs when the involution of the uterus after delivery is impaired or delayed. Breast engorgement is swelling of the breasts due to increased blood and lymph supply before lactation begins.
3. Mastitis is an inflammation of the breast tissue that is usually caused by bacterial infection during breastfeeding. Left untreated it can develop into a breast abscess, which is a localized collection of pus in the breast that requires drainage.