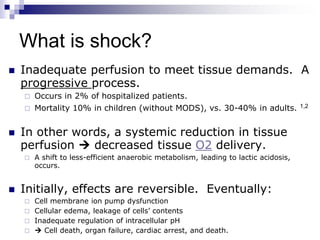
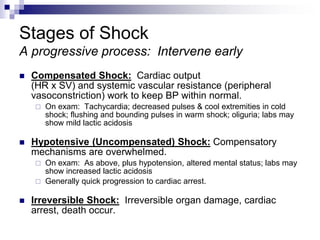
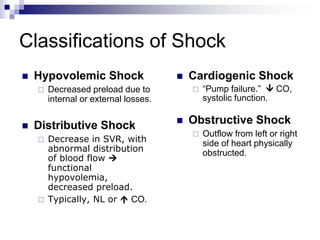
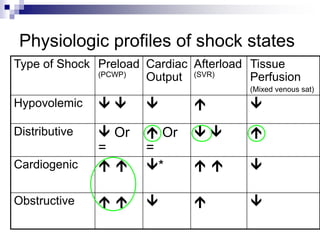
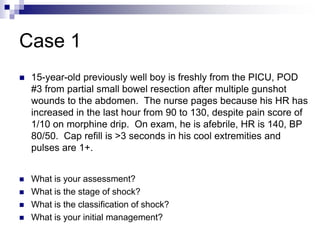
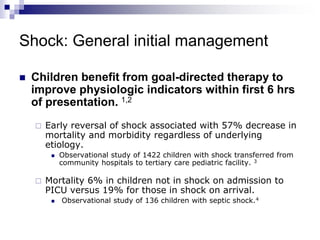
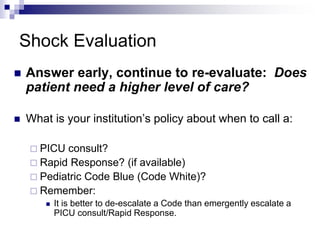
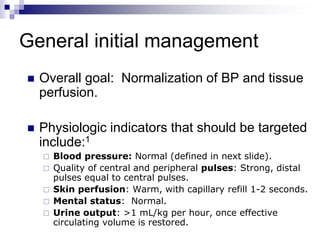
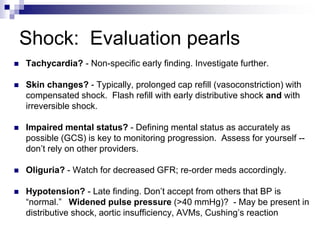
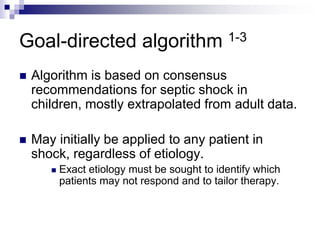
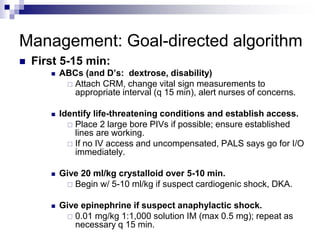
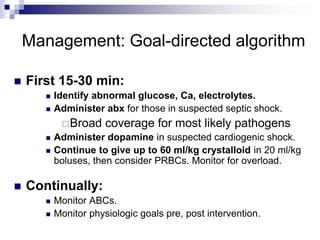
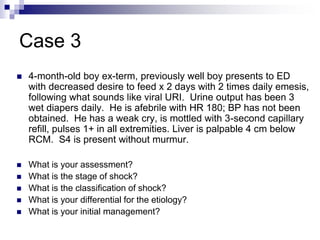
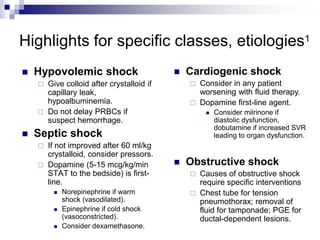
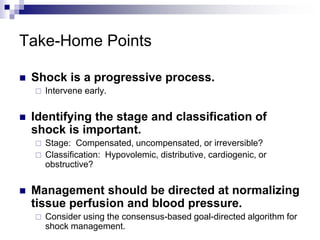
This document provides an overview of pediatric shock, including definitions, stages, classifications, signs and symptoms, differential diagnoses, and initial management strategies. It emphasizes the importance of early intervention and goal-directed therapy. Shock is defined as inadequate perfusion to meet tissue demands and can be classified as hypovolemic, distributive, cardiogenic, or obstructive. The stages include compensated, uncompensated, and irreversible. Initial management involves stabilizing vital functions, identifying shock type and etiology, providing IV fluids and vasoactive medications, and monitoring for normalization of blood pressure and perfusion.